Hip Pelvis.
2015 Dec;27(4):223-231. 10.5371/hp.2015.27.4.223.
Cementless Revision Total Hip Arthroplasty with Ceramic Articulation
- Affiliations
-
- 1Department of Orthopedic Surgery, Inha University School of Medicine, Incheon, Korea. moon@inha.ac.kr
- KMID: 2150510
- DOI: http://doi.org/10.5371/hp.2015.27.4.223
Abstract
- PURPOSE
The results of ceramic-on-ceramic (CoC) bearing surfaces in primary total hip arthroplasty (THA) were well known. However, it was not known in revision THA. The purpose of this study is to report the results of revision THA with ceramic articulation.
MATERIALS AND METHODS
A total of 112 revision THAs were evaluated. The mean age at the time of surgery was 51.6 years (27.7 to 84.2 years). The mean duration of the follow-up periods was 6.3 years (2.3 to 11.4 years).
RESULTS
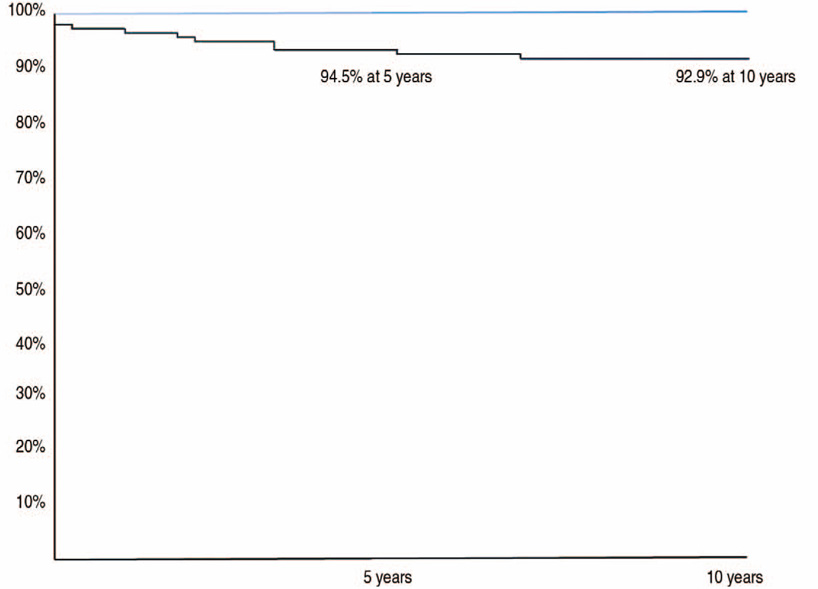
The Harris hip scores improved from an average of 56.2 at the index surgery to an average of 93.3 at the last follow-up (P<0.001). None of hips showed osteolysis or ceramic head fracture. One hip showed aseptic loosening in the acetabular component with squeaking that caused a re-revision. There were nine cases of dislocation. The survivorship at 5 years was 94.5% (95% confidence interval, 87.9% to 97.6%) with revision for any reason as the endpoint and 100% with femoral revision.
CONCLUSION
The ceramic articulation is one of good bearing options for revision THA in patients with a long life expectancy.
MeSH Terms
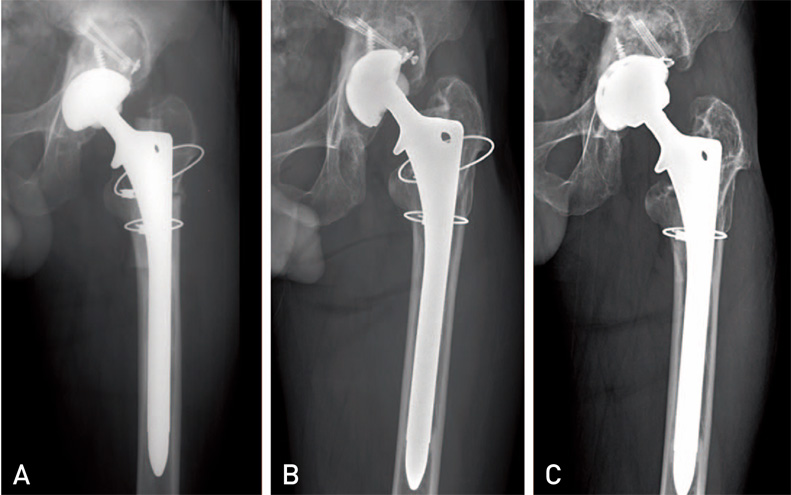
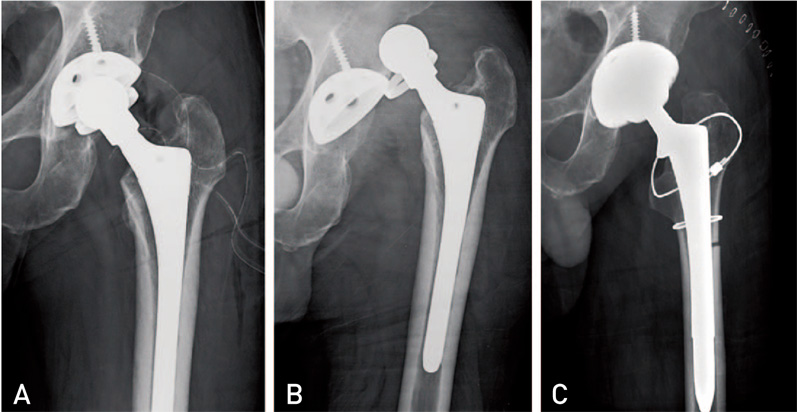
Figure
Reference
-
1. Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005; 87:1487–1497.
Article2. Ulrich SD, Seyler TM, Bennett D, et al. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008; 32:597–604.
Article3. Pospischill M, Knahr K. Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem. Follow-up for ten to 17 years. J Bone Joint Surg Br. 2005; 87:1210–1215.4. Zichner L, Lindenfeld T. In-vivo wear of the slide combinations ceramics-polyethylene as opposed to metal-polyethylene. Orthopade. 1997; 26:129–134.5. Amstutz HC, Campbell P, Kossovsky N, Clarke IC. Mechanism and clinical significance of wear debris-induced osteolysis. Clin Orthop Relat Res. 1992; (276):7–18.
Article6. Brodner W, Bitzan P, Meisinger V, Kaider A, Gottsauner-Wolf F, Kotz R. Serum cobalt levels after metal-on-metal total hip arthroplasty. J Bone Joint Surg Am. 2003; 85-A:2168–2173.
Article7. Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am. 2001; 83-A:428–436.
Article8. Jack CM, Molloy DO, Walter WL, Zicat BA, Walter WK. The use of ceramic-on-ceramic bearings in isolated revision of the acetabular component. Bone Joint J. 2013; 95-B:333–338.
Article9. Pospischill M, Knahr K. Strategies for head and inlay exchange in revision hip arthroplasty. Int Orthop. 2011; 35:261–265.
Article10. Paprosky WG, Burnett RS. Assessment and classification of bone stock deficiency in revision total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2002; 31:459–464.11. Williams VG 2nd, Whiteside LA, White SE, McCarthy DS. Fixation of ultrahigh-molecular-weight polyethylene liners to metal-backed acetabular cups. J Arthroplasty. 1997; 12:25–31.
Article12. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.
Article13. Jasty M, Harris WH. Salvage total hip reconstruction in patients with major acetabular bone deficiency using structural femoral head allografts. J Bone Joint Surg Br. 1990; 72:63–67.
Article14. Cadambi A, Engh GA, Dwyer KA, Vinh TN. Osteolysis of the distal femur after total knee arthroplasty. J Arthroplasty. 1994; 9:579–594.
Article15. revisan C, Nava V, Mattavelli M, Parra CG. Bisphosphonate treatment for osteolysis in total hip arthroplasty. A report of four cases. Clin Cases Miner Bone Metab. 2013; 10:61–64.16. Tamaki Y, Goto T, Hamada D, et al. Massive femoral osteolysis secondary to loosening of a cemented roughened long stem: a case report. Case Rep Orthop. 2014; 2014:840267.
Article17. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.
Article18. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990; (257):107–128.
Article19. Melloh M, Eggli S, Busato A, Roder C. Predictors of early stem loosening after total hip arthroplasty: a case-control study. J Orthop Surg (Hong Kong). 2011; 19:269–273.
Article20. Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978; 60:217–220.
Article21. Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982; 64:1295–1306.
Article22. Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT. Femoral anteversion. J Bone Joint Surg Am. 1987; 69:1169–1176.
Article23. Renkawitz T, Sendtner E, Schuster T, Weber M, Grifka J, Woerner M. Femoral pinless length and offset measurements during computer-assisted, minimally invasive total hip arthroplasty. J Arthroplasty. 2014; 29:1021–1025.
Article24. Murray DW, Carr AJ, Bulstrode C. Survival analysis of joint replacements. J Bone Joint Surg Br. 1993; 75:697–704.
Article25. Han CD, Choe WS, Yoo JH. Effect of polyethylene wear on osteolysis in cementless primary total hip arthroplasty: minimal 5-year follow-up study. J Arthroplasty. 1999; 14:714–723.
Article26. Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009; 91:451–458.27. Bierbaum BE, Nairus J, Kuesis D, Morrison JC, Ward D. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res. 2002; (405):158–163.
Article28. Chang JD, Kamdar R, Yoo JH, Hur M, Lee SS. Third-generation ceramic-on-ceramic bearing surfaces in revision total hip arthroplasty. J Arthroplasty. 2009; 24:1231–1235.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-term Results of Cementless Ceramic-on-ceramic Articulation Total Hip Arthroplasty
- Short-term Results of Cementless Total Hip Arthroplasty Using Ceramic on Ceramic Articulation
- Failure of a Metal Femoral Head after Revision Total Hip Arthroplasty for a Ceramic Liner Fracture
- Ceramic Head Fracture in Ceramic-on-Polyethylene Total Hip Arthroplasty
- Cementless Total Hip Arthroplasty Using a Ceramic on Ceramic Bearing Surface: The Clinical Results of a Minimum 10-year Follow-up for Patients with Short Term Follow-up