J Korean Surg Soc.
2013 Feb;84(2):107-113. 10.4174/jkss.2013.84.2.107.
The occlusion rate and patterns of saphenous vein after radiofrequency ablation
- Affiliations
-
- 1Department of Surgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea. jhjoh@khu.ac.kr
- KMID: 2144998
- DOI: http://doi.org/10.4174/jkss.2013.84.2.107
Abstract
- PURPOSE
Radiofrequency ablation (RFA) is a widely accepted to treat the varicose vein. However, outcome studies for occlusion rate and patterns of the saphenous vein after RFA are scarce. The purpose of our study is to report the results of RFA in patients with varicose vein.
METHODS
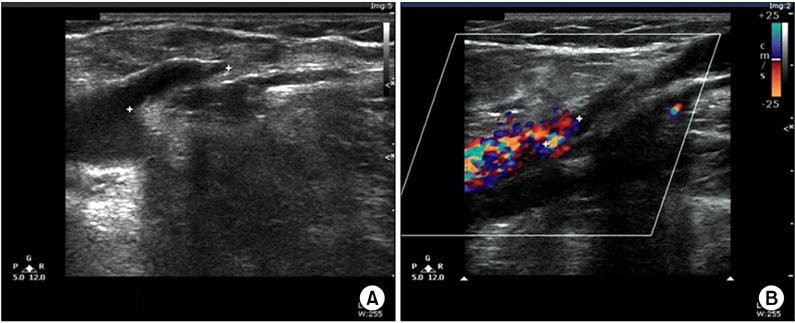
We retrospectively reviewed the clinical outcomes after RFA using ClosureFAST (Covidien) catheter. We evaluated the occlusion rate and patterns with duplex scanning after RFA.
RESULTS
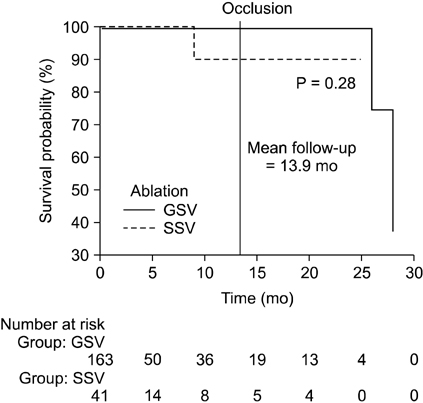
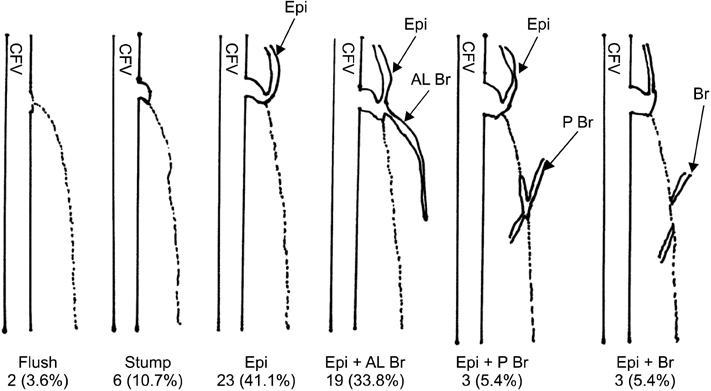
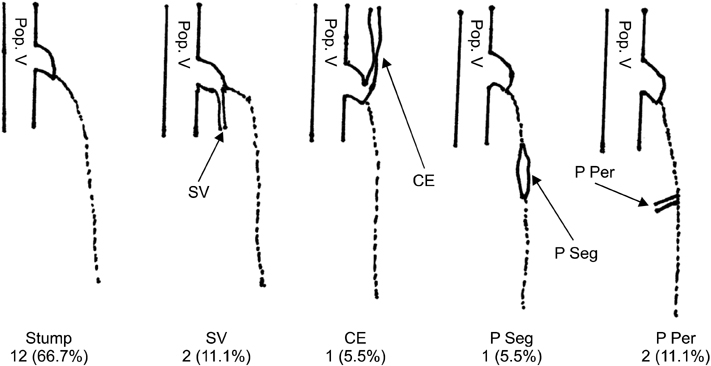
A total of 200 limbs (148 patients) underwent RFA. The truncal veins were ablated in 163 great saphenous veins (GSV) and 41 small saphenous veins (SSVs). The mean age was 52.1 +/- 11.9 years and female to male ratio was 125 : 87. At the mean follow-up of 13.9 months, the CEAP score, VCSS, and QoL score were significantly improved 2.33 +/- 0.78 to 1.29 +/- 0.96 (P < 0.0001), 3.48 +/- 0.98 to 0.63 +/- 1.16 (P < 0.0001), and 6.91 +/- 6.69 to 3.38 +/- 4.74 (P < 0.0001), respectively. The occlusion rate was 94.6% (53/56) in GSV and 94.5% (17/18) in SSV. The most common occlusion pattern in GSV was total occlusion of main trunk with patent superficial inferior epigastric vein in 41.1%. And, the most common pattern in SSV was the total occlusion of SSV with stump in 66.7%.
CONCLUSION
RFA is an effective modality in the treatment of varicose vein. At the mean follow-up of 13.9 months, the occlusion rate was 94.6%in GSV and 94.5% in SSV. There are several patterns of saphenous occlusion after RFA.
MeSH Terms
Figure
Reference
-
1. Lohr J, Kulwicki A. Radiofrequency ablation: evolution of a treatment. Semin Vasc Surg. 2010. 23:90–100.2. Carradice D, Mekako AI, Mazari FA, Samuel N, Hatfield J, Chetter IC. Randomized clinical trial of endovenous laser ablation compared with conventional surgery for great saphenous varicose veins. Br J Surg. 2011. 98:501–510.3. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011. 98:1079–1087.4. Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, Gloviczki ML, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011. 53:5 Suppl. 2S–48S.5. Goode SD, Chowdhury A, Crockett M, Beech A, Simpson R, Richards T, et al. Laser and radiofrequency ablation study (LARA study): a randomised study comparing radiofrequency ablation and endovenous laser ablation (810 nm). Eur J Vasc Endovasc Surg. 2010. 40:246–253.6. Nordon IM, Hinchliffe RJ, Brar R, Moxey P, Black SA, Thompson MM, et al. A prospective double-blind randomized controlled trial of radiofrequency versus laser treatment of the great saphenous vein in patients with varicose veins. Ann Surg. 2011. 254:876–881.7. Garratt AM, Macdonald LM, Ruta DA, Russell IT, Buckingham JK, Krukowski ZH. Towards measurement of outcome for patients with varicose veins. Qual Health Care. 1993. 2:5–10.8. Vasquez MA, Rabe E, McLafferty RB, Shortell CK, Marston WA, Gillespie D, et al. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. 2010. 52:1387–1396.9. Merchant RF, DePalma RG, Kabnick LS. Endovascular obliteration of saphenous reflux: a multicenter study. J Vasc Surg. 2002. 35:1190–1196.10. Perrin MR, Guex JJ, Ruckley CV, dePalma RG, Royle JP, Eklof B, et al. REVAS group. Recurrent varices after surgery (REVAS), a consensus document. Cardiovasc Surg. 2000. 8:233–245.11. Helmy ElKaffas K, ElKashef O, ElBaz W. Great saphenous vein radiofrequency ablation versus standard stripping in the management of primary varicose veins-a randomized clinical trial. Angiology. 2011. 62:49–54.12. Proebstle TM, Alm J, Gockeritz O, Wenzel C, Noppeney T, Lebard C, et al. Three-year European follow-up of endovenous radiofrequency-powered segmental thermal ablation of the great saphenous vein with or without treatment of calf varicosities. J Vasc Surg. 2011. 54:146–152.13. Labropoulos N, Leon M, Nicolaides AN, Giannoukas AD, Volteas N, Chan P. Superficial venous insufficiency: correlation of anatomic extent of reflux with clinical symptoms and signs. J Vasc Surg. 1994. 20:953–958.14. Delis KT, Knaggs AL, Khodabakhsh P. Prevalence, anatomic patterns, valvular competence, and clinical significance of the Giacomini vein. J Vasc Surg. 2004. 40:1174–1183.15. Marsh P, Price BA, Holdstock J, Harrison C, Whiteley MS. Deep vein thrombosis (DVT) after venous thermoablation techniques: rates of endovenous heat-induced thrombosis (EHIT) and classical DVT after radiofrequency and endovenous laser ablation in a single centre. Eur J Vasc Endovasc Surg. 2010. 40:521–527.16. Mozes G, Kalra M, Carmo M, Swenson L, Gloviczki P. Extension of saphenous thrombus into the femoral vein: a potential complication of new endovenous ablation techniques. J Vasc Surg. 2005. 41:130–135.17. Lawrence PF, Chandra A, Wu M, Rigberg D, DeRubertis B, Gelabert H, et al. Classification of proximal endovenous closure levels and treatment algorithm. J Vasc Surg. 2010. 52:388–393.18. Manfrini S, Gasbarro V, Danielsson G, Norgren L, Chandler JG, Lennox AF, et al. Endovenous Reflux Management Study Group. Endovenous management of saphenous vein reflux. J Vasc Surg. 2000. 32:330–342.19. Hingorani AP, Ascher E, Markevich N, Schutzer RW, Kallakuri S, Hou A, et al. Deep venous thrombosis after radiofrequency ablation of greater saphenous vein: a word of caution. J Vasc Surg. 2004. 40:500–504.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Saphenous vein occlusion with cyanoacrylate: a systematic review
- Effect of Diameter of Saphenous Vein on Stump Length after Radiofrequency Ablation for Varicose Vein
- Short-Term Results of Radiofrequency Thermal Ablation Using VENISTAR Ⓡ in Treatment of Varicose Veins
- The Early Results of Endovenous Radiofrequency Ablation Combined with Flush High Ligation for Patients with Varicose Veins
- The Effect of Saphenous Vein Ablation on Combined Segmental Popliteal Vein Reflux