J Cardiovasc Ultrasound.
2015 Mar;23(1):27-31. 10.4250/jcu.2015.23.1.27.
Superior Vena Cava Echocardiography as a Screening Tool to Predict Cardiovascular Implantable Electronic Device Lead Fibrosis
- Affiliations
-
- 1Department of Medicine, Drexel University College of Medicine, Philadelphia, PA, USA.
- 2Department of Medicine, Division of Cardiology, Drexel University College of Medicine, Philadelphia, PA, USA. Andrew.Kohut@drexelmed.edu
- KMID: 2135403
- DOI: http://doi.org/10.4250/jcu.2015.23.1.27
Abstract
- BACKGROUND
Currently there is no noninvasive imaging modality used to risk stratify patients requiring lead extractions. We report the novel use of superior vena cava (SVC) echocardiography to identify lead fibrosis and complex cardiac implantable electronic device (CIED) lead extraction. With an aging population and expanding indications for cardiac device implantation, the ability to deal with the complications associated with chronically implanted device has also increased.
METHODS
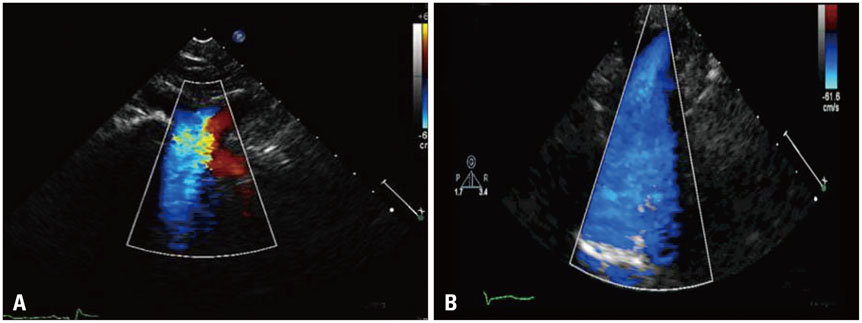
This was a retrospective analysis of Doppler echocardiography recorded in our outpatient Electrophysiology/Device Clinic office over 6 months. Images from 109 consecutive patients were reviewed.
RESULTS
62% (68/109) did not have a CIED and 38% (41/109) had a CIED. In patients without a CIED, 6% (4/68) displayed turbulent color flow by Doppler in the SVC, while 22% (9/41) of patients with a CIED displayed turbulent flow. Fisher's exact test found a statistically significant difference between the two groups (p value < 0.05). The CIED group was subdivided into 2 groups based on device implant duration (< 2 years vs. > or = 2 years). Of the CIED implanted for > or = 2 years, 27% (9/33) had turbulent flow in the SVC by Doppler, while no patients (0/8) with implant durations < 2 years demonstrated turbulent flow. Nine patients underwent subsequent lead extraction. A turbulent color pattern successfully identified all 3 patients that had significant fibrosis in the SVC found during extraction.
CONCLUSION
Our data suggests that assessing turbulent flow using color Doppler in the SVC may be a valuable noninvasive screening tool prior to lead extraction in predicting complex procedures.
MeSH Terms
Figure
Reference
-
1. Kurtz SM, Ochoa JA, Lau E, Shkolnikov Y, Pavri BB, Frisch D, Greenspon AJ. Implantation trends and patient profiles for pacemakers and implantable cardioverter defibrillators in the United States: 1993-2006. Pacing Clin Electrophysiol. 2010; 33:705–711.2. Wilkoff BL, Love CJ, Byrd CL, Bongiorni MG, Carrillo RG, Crossley GH 3rd, Epstein LM, Friedman RA, Kennergren CE, Mitkowski P, Schaerf RH, Wazni OM. Heart Rhythm Society. American Heart Association. Transvenous lead extraction: Heart Rhythm Society expert consensus on facilities, training, indications, and patient management: this document was endorsed by the American Heart Association (AHA). Heart Rhythm. 2009; 6:1085–1104.3. Love CJ, Wilkoff BL, Byrd CL, Belott PH, Brinker JA, Fearnot NE, Friedman RA, Furman S, Goode LB, Hayes DL, Kawanishi DT, Parsonnet V, Reiser C, Van Zandt HJ. Recommendations for extraction of chronically implanted transvenous pacing and defibrillator leads: indications, facilities, training. North American Society of Pacing and Electrophysiology Lead Extraction Conference Faculty. Pacing Clin Electrophysiol. 2000; 23(4 Pt 1):544–551.4. Kutalek SP. Pacemaker and defibrillator lead extraction. Curr Opin Cardiol. 2004; 19:19–22.5. Hauser RG, Katsiyiannis WT, Gornick CC, Almquist AK, Kallinen LM. Deaths and cardiovascular injuries due to device-assisted implantable cardioverter-defibrillator and pacemaker lead extraction. Europace. 2010; 12:395–401.6. Smith HJ, Fearnot NE, Byrd CL. Where does scar tissue form to inhibit extraction of chronic pacemaker leads (Abstract). J Am Coll Cardiol. 1992; 19:148A.7. Lo R, D'Anca M, Cohen T, Kerwin T. Incidence and prognosis of pacemaker lead-associated masses: a study of 1,569 transesophageal echocardiograms. J Invasive Cardiol. 2006; 18:599–601.8. Bongiorni MG, Di Cori A, Soldati E, Zucchelli G, Arena G, Segreti L, De Lucia R, Marzilli M. Intracardiac echocardiography in patients with pacing and defibrillating leads: a feasibility study. Echocardiography. 2008; 25:632–638.9. Bulur S, Vural A, Yazıcı M, Ertaş G, Özhan H, Ural D. Incidence and predictors of subclavian vein obstruction following biventricular device implantation. J Interv Card Electrophysiol. 2010; 29:199–202.10. Korkeila P, Mustonen P, Koistinen J, Nyman K, Ylitalo A, Karjalainen P, Lund J, Airaksinen J. Clinical and laboratory risk factors of thrombotic complications after pacemaker implantation: a prospective study. Europace. 2010; 12:817–824.11. Korkeila P, Ylitalo A, Koistinen J, Airaksinen KE. Progression of venous pathology after pacemaker and cardioverter-defibrillator implantation: a prospective serial venographic study. Ann Med. 2009; 41:216–223.12. Khouzam RN, Minderman D, D'Cruz IA. Echocardiography of the superior vena cava. Clin Cardiol. 2005; 28:362–366.13. Cohen ML, Cohen BS, Kronzon I, Lighty GW, Winer HE. Superior vena caval blood flow velocities in adults: a Doppler echocardiographic study. J Appl Physiol (1985). 1986; 61:215–219.14. Nishino M, Tanouchi J, Ito T, Tanaka K, Aoyama T, Kitamura M, Nakagawa T, Kato J, Yamada Y. Echographic detection of latent severe thrombotic stenosis of the superior vena cava and innominate vein in patients with a pacemaker: integrated diagnosis using sonography, pulse Doppler, and color flow. Pacing Clin Electrophysiol. 1997; 20(4 Pt 1):946–952.15. Hammerli M, Meyer RA. Doppler evaluation of central venous lines in the superior vena cava. J Pediatr. 1993; 122:S104–S108.16. Kohut AR, Grammes J, Schulze CM, Al-Bataineh M, Yesenosky GA, Horrow JC, Kutalek SP. Percutaneous extraction of ePTFE-coated ICD leads: a single center comparative experience. Pacing Clin Electrophysiol. 2013; 36:444–450.17. Maytin M, Epstein LM, John RM. Lead implant duration does not always predict ease of extraction: extraction sheath may be required at < 1 year. Pacing Clin Electrophysiol. 2011; 34:1615–1620.18. Jones SO 4th, Eckart RE, Albert CM, Epstein LM. Large, single-center, single-operator experience with transvenous lead extraction: outcomes and changing indications. Heart Rhythm. 2008; 5:520–525.19. Farooqi FM, Talsania S, Hamid S, Rinaldi CA. Extraction of cardiac rhythm devices: indications, techniques and outcomes for the removal of pacemaker and defibrillator leads. Int J Clin Pract. 2010; 64:1140–1147.20. Smith MC, Love CJ. Extraction of transvenous pacing and ICD leads. Pacing Clin Electrophysiol. 2008; 31:736–752.21. Bracke F, Meijer A, Van Gelder B. Extraction of pacemaker and implantable cardioverter defibrillator leads: patient and lead characteristics in relation to the requirement of extraction tools. Pacing Clin Electrophysiol. 2002; 25:1037–1040.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Congenital Absence of Superior Vena Cava with no Manifestation of Superior Vena Cava Syndrome
- Successful Implantation of an Implantable Cardioverter-Defibrillator Through a Persistent Left Superior Vena Cava
- Two Cases of Transhepatic Implantation of Cardiac Implantable Electronic Device: All Roads lead to Rome
- A Case of Persistent Left Superior Vena Cava with Interruption of Inferior Vena Cava
- A Case of Superior Vena Cava Syndrome