J Korean Foot Ankle Soc.
2015 Dec;19(4):188-192. 10.14193/jkfas.2015.19.4.188.
Analysis of Heel Pad Thickness in Korean
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonbuk National University Medical School, Jeonju, Korea. osdr2815@naver.com
- 2Department of Orthopedic Surgery and Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2132463
- DOI: http://doi.org/10.14193/jkfas.2015.19.4.188
Abstract
- PURPOSE
The purpose of this study is to provide Korean data on heel pad thickness according to age, gender, underlying disease, occupation, and body mass index (BMI).
MATERIALS AND METHODS
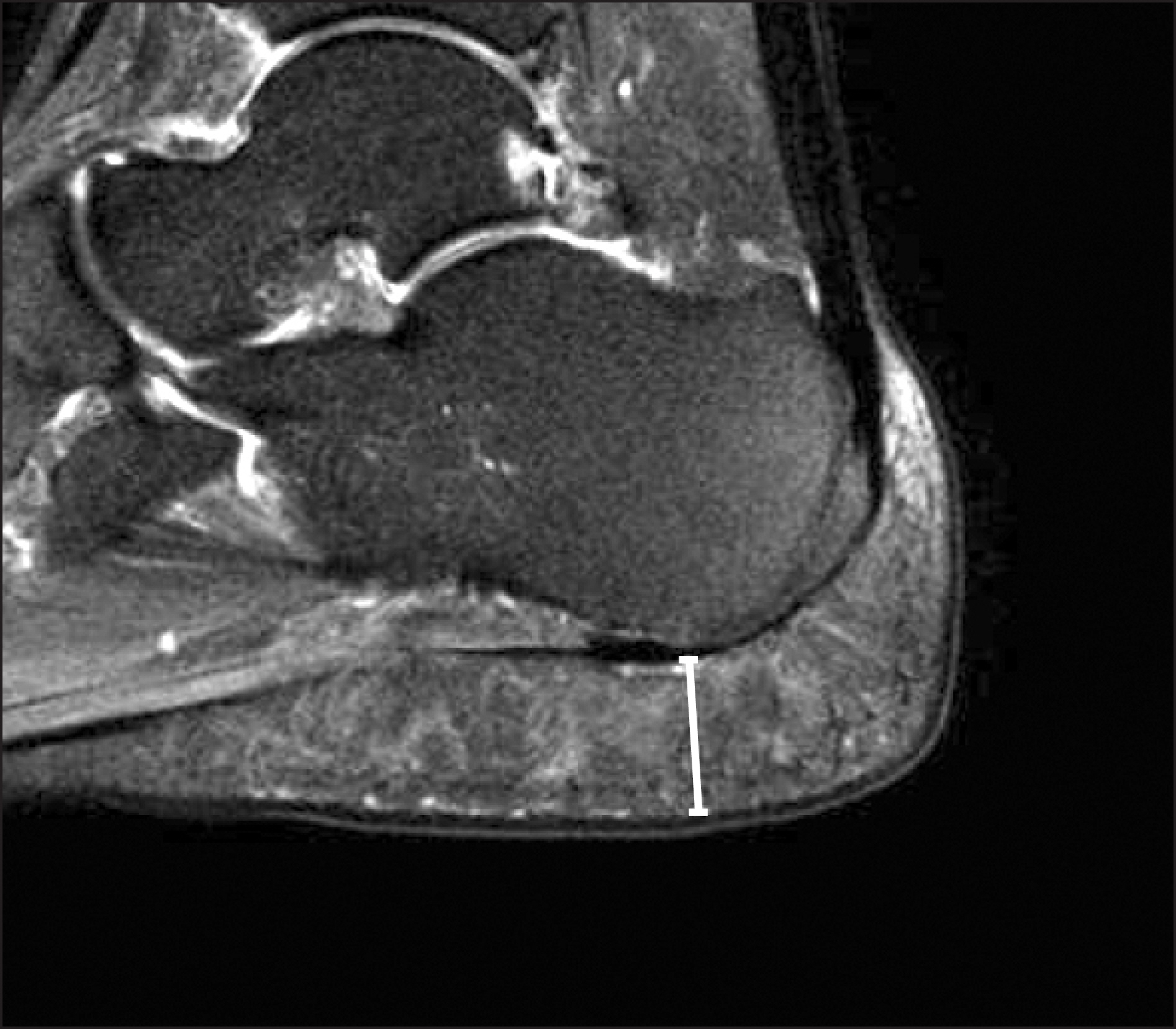
A retrospective study was conducted on 670 patients who underwent foot lateral plain radiography and magnetic resonance imaging (MRI) between January 2010 and July 2014. Through measurements of heel pad thickness, the usefulness and accuracy of foot lateral plain radiography was evaluated, and the mean Korean heel pad thickness in the weight-bearing and non-weight-bearing conditions was also evaluated according to age, gender, underlying disease, occupation, and BMI.
RESULTS
The 670 subjects with a mean age of 44 years (range, 12 to 84 years) consisted of 420 males and 250 females. The difference in heel pad thickness between non-weight-bearing foot lateral plain radiography and MRI was 0.69 mm. The heel pad thickness did not show a significant difference with age (p=0.08) and the presence of diabetes (p=0.09). With the increase in the Tegner score, the thickness of the heel pad increased (p=0.035), and subjects with a higher BMI had a thicker heel pad (p=0.03). The compressibility of the heel pad thickness showed no correlation with gender, diabetes, and Tegner score. Compressibility also increased with the increase in age and body weight.
CONCLUSION
The mean Korean heel pad thickness measured through non-weight-bearing foot lateral plain radiography was 18.79 mm. The heel pad thickness increased with increasing BMI; however, age and diabetes did not show significant correlation. The compressibility of heel pad increased with the increase in age.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Karr SD. Subcalcaneal heel pain. Orthop Clin North Am. 1994; 25:161–75.
Article2. Buschmann WR, Jahss MH, Kummer F, Desai P, Gee RO, Ricci JL. Histology and histomorphometric analysis of the normal and atrophic heel fat pad. Foot Ankle Int. 1995; 16:254–8.
Article3. Jahss MH, Michelson JD, Desai P, Kaye R, Kummer F, Buschman W, et al. Investigations into the fat pads of the sole of the foot: anatomy and histology. Foot Ankle. 1992; 13:233–42.
Article4. Hill JJ Jr, Cutting PJ. Heel pain and body weight. Foot Ankle. 1989; 9:254–6.
Article5. Prichasuk S, Mulpruek P, Siriwongpairat P. The heel-pad compressibility. Clin Orthop Relat Res. 1994; 300:197–200.
Article6. Prichasuk S, Subhadrabandhu T. The relationship of pes planus and calcaneal spur to plantar heel pain. Clin Orthop Relat Res. 1994; 306:192–6.7. Rome K, Campbell R, Flint A, Haslock I. Heel pad thickness: a contributing factor associated with plantar heel pain in young adults. Foot Ankle Int. 2002; 23:142–7.8. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985; 198:43–9.
Article9. Turgut A, Göktürk E, Köse N, Seber S, Hazer B, Günal I. The relationship of heel pad elasticity and plantar heel pain. Clin Orthop Relat Res. 1999; 360:191–6.
Article10. Steinbach HL, Russell W. Measurement of the heel-pad as an aid to diagnosis of acromegaly. Radiology. 1964; 82:418–23.
Article11. Gooding GA, Stess RM, Graf PM, Moss KM, Louie KS, Grunfeld C. Sonography of the sole of the foot. Evidence for loss of foot pad thickness in diabetes and its relationship to ulceration of the foot. Invest Radiol. 1986; 21:45–8.12. Kuhns JG. Changes in elastic adipose tissue. J Bone Joint Surg Am1. 1949; 31A:541–7.
Article13. Waldecker U, Lehr HA. Is there histomorphological evidence of plantar metatarsal fat pad atrophy in patients with diabetes? J Foot Ankle Surg. 2009; 48:648–52.14. Robertson DD, Mueller MJ, Smith KE, Commean PK, Pilgram T, Johnson JE. Structural changes in the forefoot of individuals with diabetes and a prior plantar ulcer. J Bone Joint Surg Am. 2002; 84:1395–404.
Article15. Snook GA, Chrisman OD. The management of subcalcaneal pain. Clin Orthop Relat Res. 1972; 82:163–8.
Article16. Miller WE. The heel pad. Am J Sports Med. 1982; 10:19–21.
Article17. Jørgensen U. Achillodynia and loss of heel pad shock absor-bency. Am J Sports Med. 1985; 13:128–32.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Heel Pad Thickness: Measurement by Simple Plain Radiography
- Ultrasonographic Compressibility of Heel Pads in Patients with Diabetes Mellitus
- The Effects of Modified Low-Dye Taping in the Patient with Heel Pad Atrophy
- Ultrasonographic Findings of Thickness and Compressibility of Heel Pads in Outpatient
- Clinical and Biomechanical Effects of Low-Dye Taping and Figure-8 Modification of Low-Dye Taping in Patients With Heel Pad Atrophy