Korean J Hepatobiliary Pancreat Surg.
2011 Aug;15(3):189-193. 10.14701/kjhbps.2011.15.3.189.
Therapeutic induction of hepatic atrophy for isolated injury of the right posterior sectoral duct following laparoscopic cholecystectomy
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery,. shwang@amc.seoul.kr
- 2Diagnostic Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2130992
- DOI: http://doi.org/10.14701/kjhbps.2011.15.3.189
Abstract
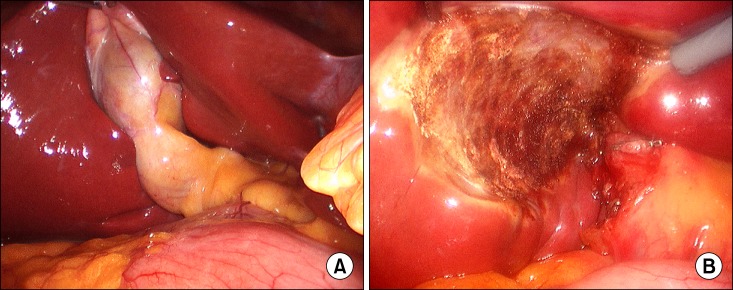
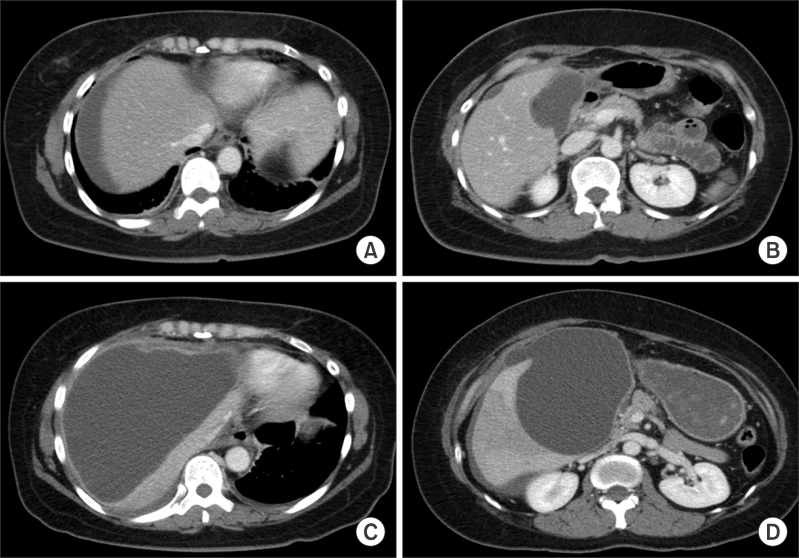
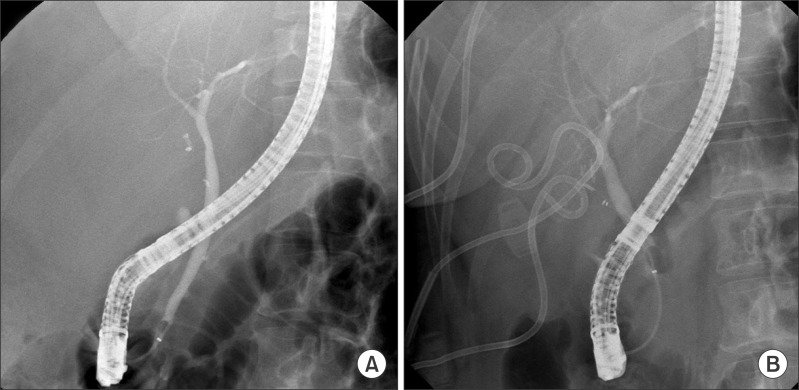
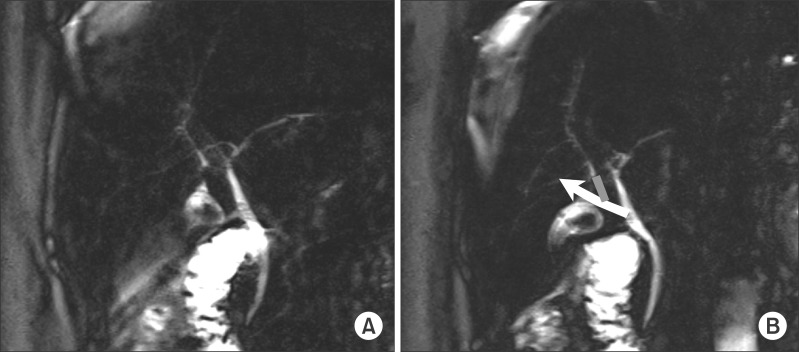
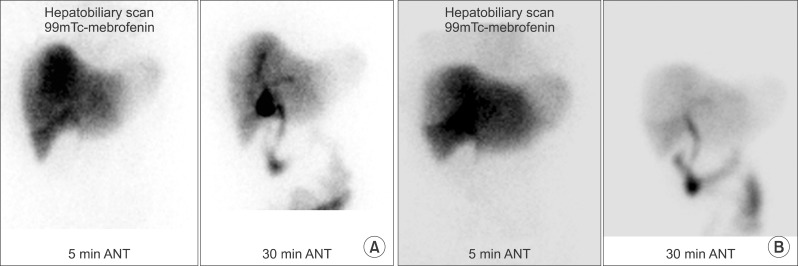
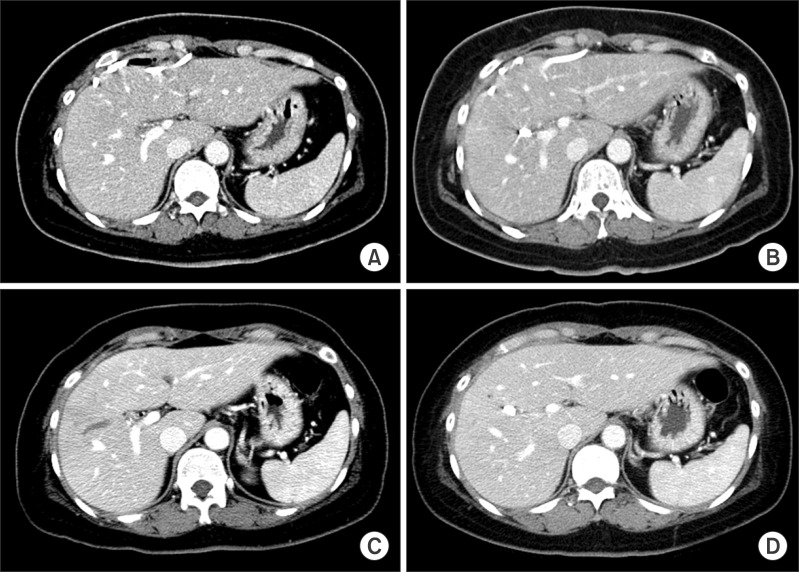
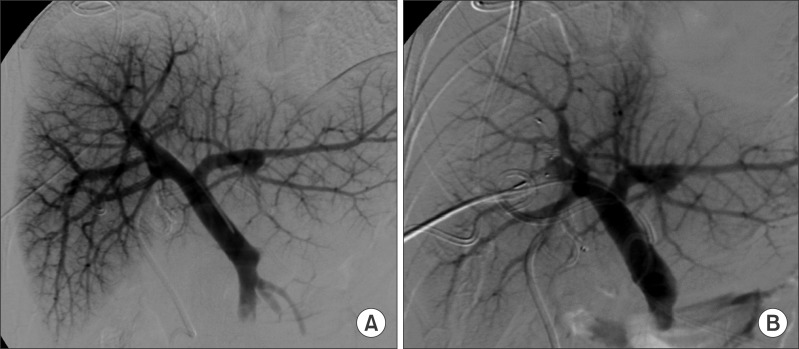
- Laparoscopic cholecystectomy has resulted in various bile duct injuries. Treatment of these injuries is usually difficult and often leads to an intractable clinical course. We herein present a case of isolated right anterior sector (RAS) duct injury induced by laparoscopic cholecystectomy. The bile duct injury was successfully treated by hepatic atrophy induction. Imaging studies revealed that the RAS duct was severed, probably due to rare anatomical variations. Considering the difficulty in surgical reconstruction, atrophy induction of the involved hepatic parenchyma was attempted. This treatment consisted of embolization of the RAS portal branch to inhibit bile production, induction of heavy adhesion at the bile leak site to ensure percutaneous pigtail clamping, and sequential clamping and removal of pigtail catheters. This procedure took 3 months prior to pigtail catheter removal. She was free from other complications during the first 12 months and to date. She will be followed up for 5 years overall including surveillance for hepatobiliary complications. Although this therapeutic induction of atrophy approach is not universally applicable, it can be considered to be a feasible option in unique situations such as this one.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Hepatic atrophy treatment with portal vein embolization to control intrahepatic duct stenosis-associated cholangitis
Shin Hwang, Gi-Young Ko, Dong-Il Gwon
Ann Hepatobiliary Pancreat Surg. 2020;24(3):339-344. doi: 10.14701/ahbps.2020.24.3.339.Necrosectomy of hepatic left lateral section after blunt abdominal trauma in a patient who underwent central hepatectomy and bile duct resection for perihilar cholangiocarcinoma
Seul Gi Oh, Shin Hwang, Suhyeon Ha, Heewon Kim, Lee Na Ryu
Ann Hepatobiliary Pancreat Surg. 2020;24(3):345-351. doi: 10.14701/ahbps.2020.24.3.345.
Reference
-
1. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125. PMID: 8000648.2. Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001; 234:549–558. PMID: 11573048.3. Sicklick JK, Camp MS, Lillemoe KD, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005; 241:786–792. PMID: 15849514.4. Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003; 237:460–469. PMID: 12677139.5. Perini RF, Uflacker R, Cunningham JT, Selby JB, Adams D. Isolated right segmental hepatic duct injury following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 2005; 28:185–195. PMID: 15770390.
Article6. Lillemoe KD, Petrofski JA, Choti MA, Venbrux AC, Cameron JL. Isolated right segmental hepatic duct injury: a diagnostic and therapeutic challenge. J Gastrointest Surg. 2000; 4:168–177. PMID: 10675240.
Article7. Kurumi Y, Tani T, Hanasawa K, Kodama M. The prevention of bile duct injury during laparoscopic cholecystectomy from the point of view of anatomic variation. Surg Laparosc Endosc Percutan Tech. 2000; 10:192–199. PMID: 10961744.
Article8. Hwang S, Lee SG, Lee YJ, Ha TY, Ko GY, Song GW. Delayed-onset isolated injury of the right posterior segment duct after laparoscopic cholecystectomy: a report of hepatic segmental atrophy induction. Surg Laparosc Endosc Percutan Tech. 2007; 17:203–205. PMID: 17581468.
Article9. Hwang S, Park GC, Yu YD, et al. Hepatic parenchymal atrophy induction for intractable segmental bile duct injury after liver resection. Hepatogastroenterology. (in press).10. Lillemoe KD, Melton GB, Cameron JL, et al. Postoperative bile duct strictures: management and outcome in the 1990s. Ann Surg. 2000; 232:430–441. PMID: 10973393.
Article11. Ragozzino A, De Ritis R, Mosca A, Iaccarino V, Imbriaco M. Value of MR cholangiography in patients with iatrogenic bile duct injury after cholecystectomy. AJR Am J Roentgenol. 2004; 183:1567–1572. PMID: 15547192.
Article12. Park MS, Kim KW, Yu JS, et al. Early biliary complications of laparoscopic cholecystectomy: evaluation on T2-weighted MR cholangiography in conjunction with mangafodipir trisodium-enhanced 3D T1-weighted MR cholangiography. AJR Am J Roentgenol. 2004; 183:1559–1566. PMID: 15547191.13. Uesaka K, Nimura Y, Nagino M. Changes in hepatic lobar function after right portal vein embolization. An appraisal by biliary indocyanine green excretion. Ann Surg. 1996; 223:77–83. PMID: 8554422.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acetic acid sclerotherapy for treatment of biliary leak from an isolated right posterior sectoral duct after cholecystectomy
- Successful non-surgical treatment for isolated right anterior section bile duct injury following laparoscopic cholecystectomy: Report of a case
- Isolated aberrant right cysticohepatic duct injury during laparoscopic cholecystectomy: Evaluation and treatment challenges of a severe postoperative complication associated with an extremely rare anatomical variant
- Erratum: Therapeutic induction of hepatic atrophy for isolated injury of the right anterior sectoral duct following laparoscopic cholecystectomy
- Cystic duct variation detected by near-infrared fluorescent cholangiography during laparoscopic cholecystectomy