Ann Hepatobiliary Pancreat Surg.
2020 May;24(2):221-227. 10.14701/ahbps.2020.24.2.221.
Isolated aberrant right cysticohepatic duct injury during laparoscopic cholecystectomy: Evaluation and treatment challenges of a severe postoperative complication associated with an extremely rare anatomical variant
- Affiliations
-
- 1First Surgical Department, General Hospital Papageorgiou, Greece
- 2Department of Radiology, General Hospital Papageorgiou, Greece
- 3School of Medicine, Aristotle University of Thessaloniki, Greece
- 4Department of Gastroenterology, General Hospital Papanikolaou, Thessaloniki, Greece
- KMID: 2500810
- DOI: http://doi.org/10.14701/ahbps.2020.24.2.221
Abstract
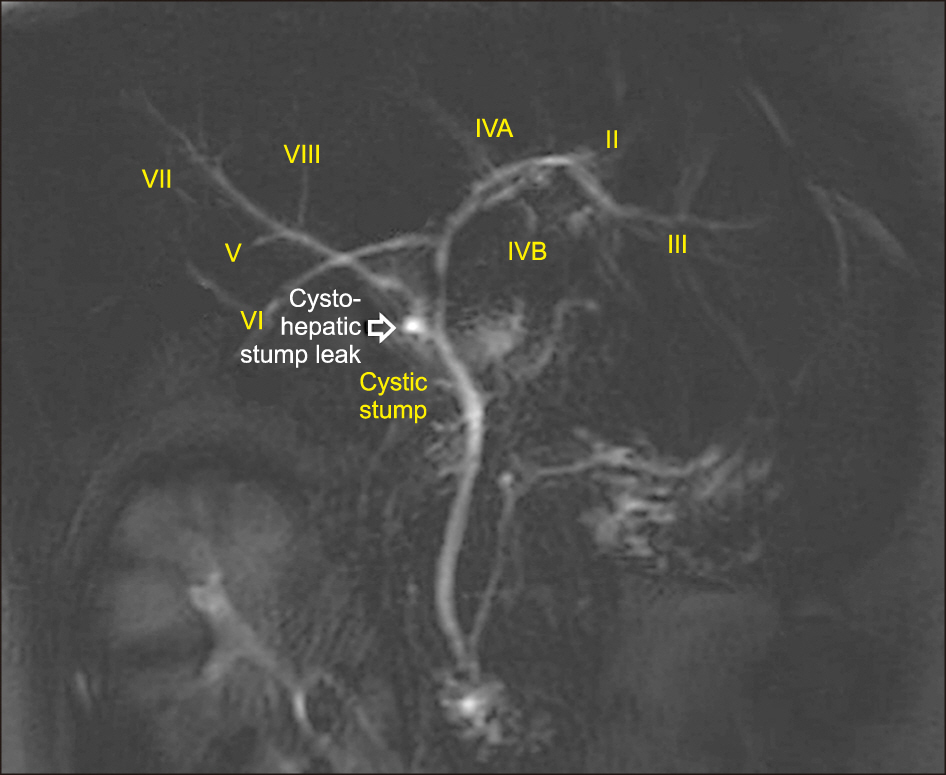
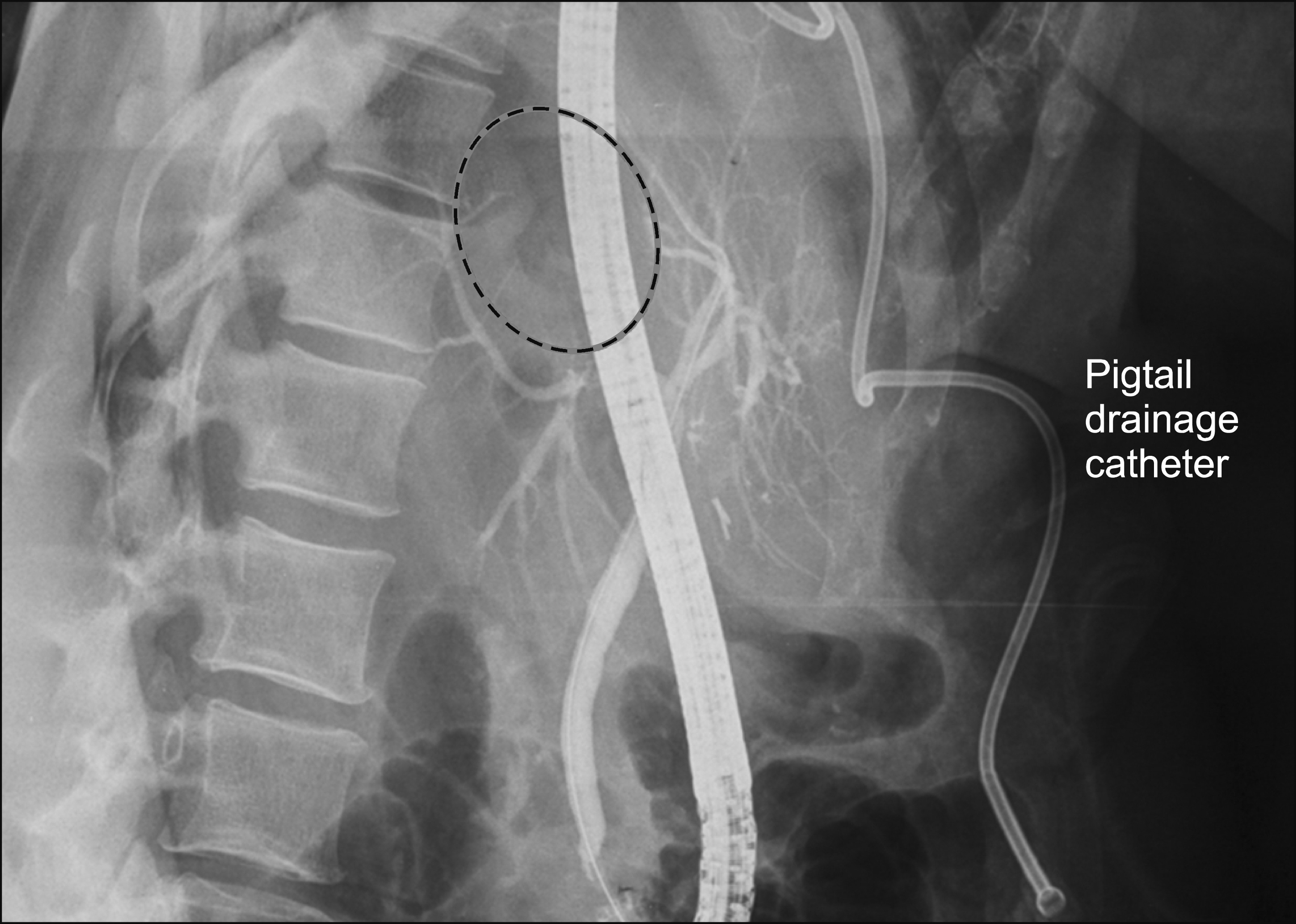
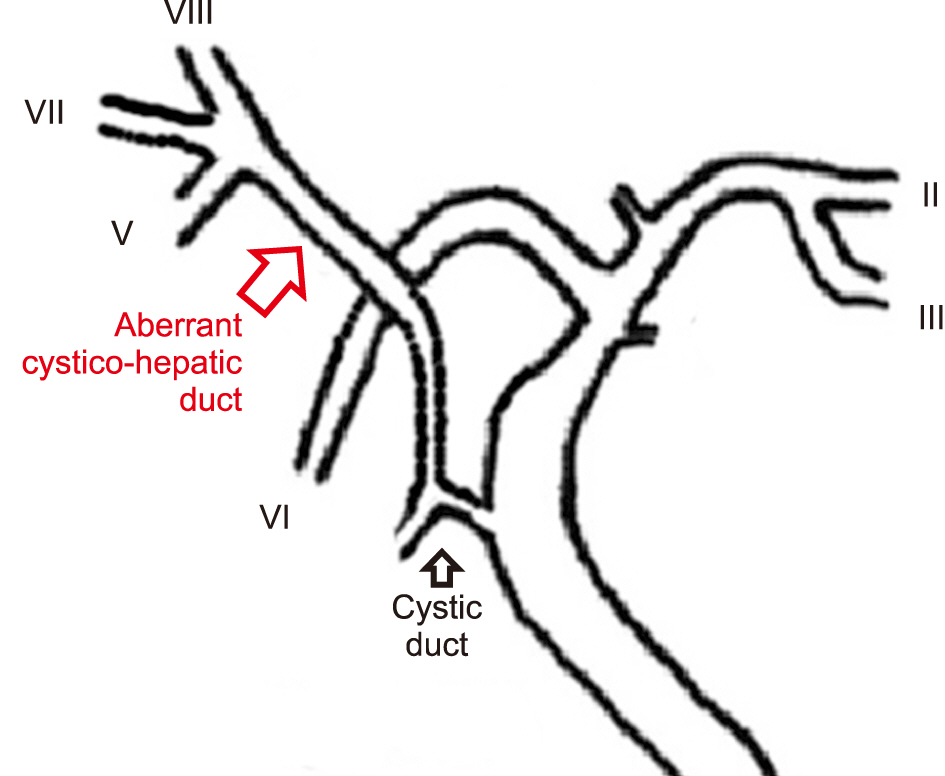
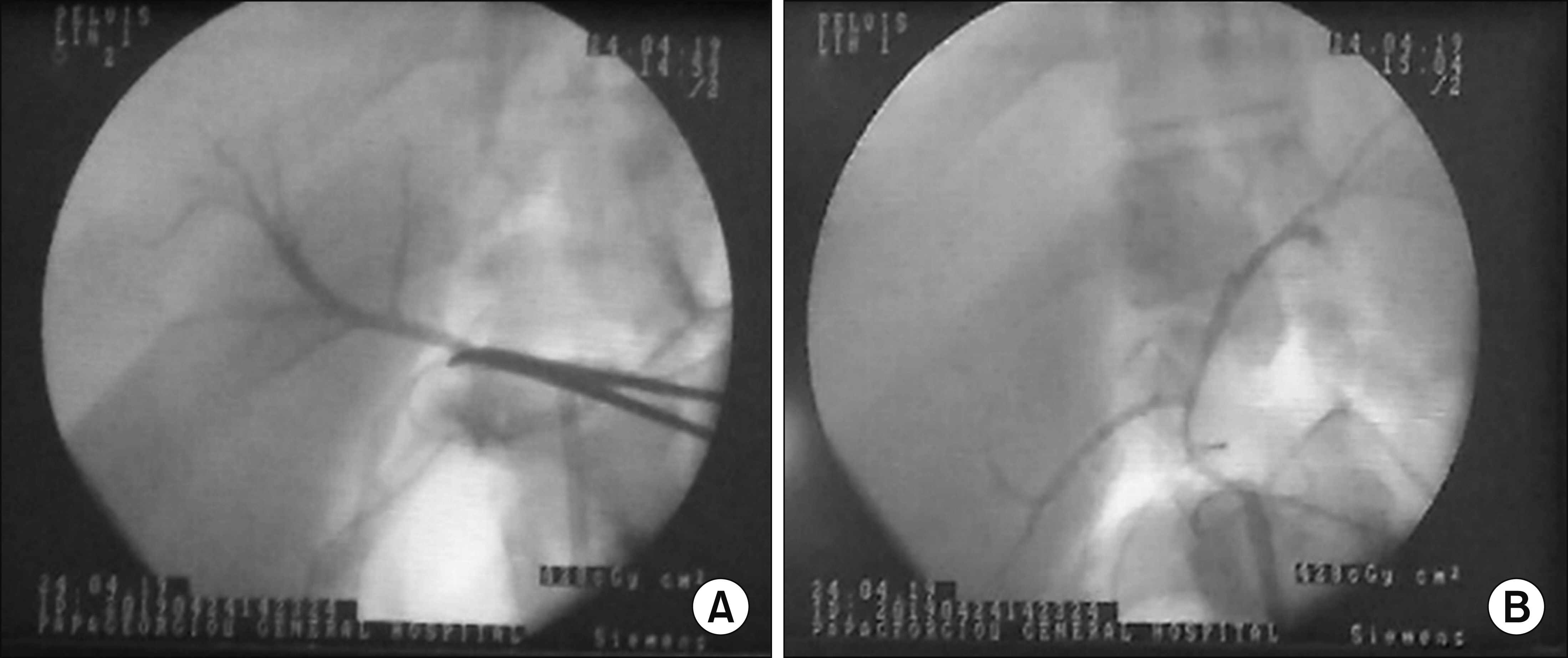
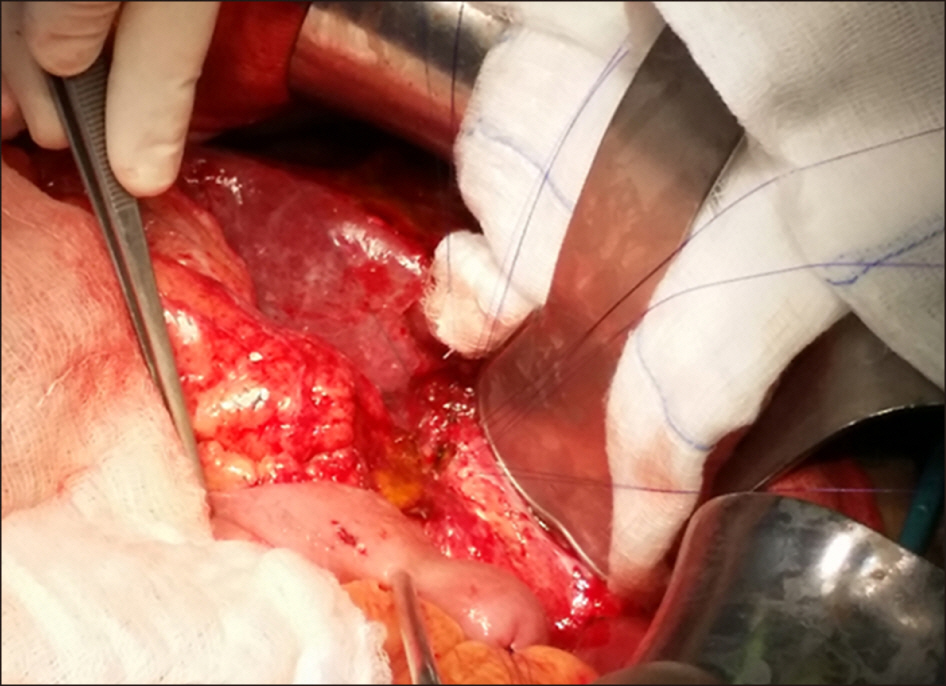
- A typical bile duct branching patterns represent one of the major causes of bile duct injury (BDI) during laparoscopic cholecystectomy (LC). The most common classified variations of bile duct branching, involve the right posterior sectoral duct (RPSD) and its joining with the right anterior or left hepatic duct. Variant bile duct anatomy can rarely be extremely complex and unclassified. This report describes an extremely rare case of an isolated injury to an aberrant right hepatic duct formed by the joining of ducts from segments V, VII, and VIII draining into the cystic duct (cysticohepatic duct) during LC, associated with an inferior RPSD opening to left hepatic duct. Detailed evaluation of both endoscopic and magnetic cholangiograms established the diagnosis. Bile duct injury was subsequently managed surgically by a demanding Roux-en-Y hepaticojejunostomy. This extremely rare case aims to serve as a useful reminder of the consistent inconsistency of biliary anatomy, alerting surgeons to beware of variant bile duct branching patterns during open or LC that constitute a dreadful pitfall for severe and life-threatening bile duct injuries.
Keyword
Figure
Reference
-
1. Mangieri CW, Hendren BP, Strode MA, Bandera BC, Faler BJ. 2019; Bile duct injuries (BDI) in the advanced laparoscopic cholecystectomy era. Surg Endosc. 33:724–730. DOI: 10.1007/s00464-018-6333-7. PMID: 30006843.
Article2. Martin RF, Rossi RL. 1994; Bile duct injuries. Spectrum, mechanisms of injury, and their prevention. Surg Clin North Am. 74:781–803. discussion 805–807. DOI: 10.1016/S0039-6109(16)46380-2. PMID: 8047942.
Article3. Sarawagi R, Sundar S, Raghuvanshi S, Gupta SK, Jayaraman G. 2016; Common and uncommon anatomical variants of intrahepatic bile ducts in magnetic resonance cholangiopancreatography and its clinical implication. Pol J Radiol. 81:250–255. DOI: 10.12659/PJR.895827. PMID: 27298653. PMCID: PMC4886616.
Article4. Choi JW, Kim TK, Kim KW, Kim AY, Kim PN, Ha HK, et al. 2003; Anatomic variation in intrahepatic bile ducts: an analysis of intraoperative cholangiograms in 300 consecutive donors for living donor liver transplantation. Korean J Radiol. 4:85–90. DOI: 10.3348/kjr.2003.4.2.85. PMID: 12845303. PMCID: PMC2698075.
Article5. Lyu SY, Pan KT, Chu SY, Hsu MY, Chen CM, Hung CF, et al. 2012; Common and rare variants of the biliary tree: magnetic resonance cholangiographic findings and clinical implications. J Radiol Sci. 37:59–67.6. Karakas HM, Celik T, Alicioglu B. 2008; Bile duct anatomy of the Anatolian Caucasian population: Huang classification revisited. Surg Radiol Anat. 30:539–545. DOI: 10.1007/s00276-008-0365-y. PMID: 18491027.
Article7. Mariolis-Sapsakos T, Kalles V, Papatheodorou K, Goutas N, Papapanagiotou I, Flessas I, et al. 2012; Anatomic variations of the right hepatic duct: results and surgical implications from a cadaveric study. Anat Res Int. 2012:838179. DOI: 10.1155/2012/838179. PMID: 23056946. PMCID: PMC3465866.
Article8. Ohkubo M, Nagino M, Kamiya J, Yuasa N, Oda K, Arai T, et al. 2004; Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg. 239:82–86. DOI: 10.1097/01.sla.0000102934.93029.89. PMID: 14685104. PMCID: PMC1356196.
Article9. Kullman E, Borch K, Lindström E, Svanvik J, Anderberg B. 1996; Value of routine intraoperative cholangiography in detecting aberrant bile ducts and bile duct injuries during laparoscopic cholecystectomy. Br J Surg. 83:171–175. DOI: 10.1002/bjs.1800830207. PMID: 8689155.
Article10. Turner MA, Fulcher AS. 2001; The cystic duct: normal anatomy and disease processes. Radiographics. 21:3–22. questionnaire 288-294.DOI: 10.1148/radiographics.21.1.g01ja093. PMID: 11158640.
Article11. Champetier J, Létoublon C, Alnaasan I, Charvin B. 1991; The cystohepatic ducts: surgical implications. Surg Radiol Anat. 13:203–211. DOI: 10.1007/BF01627988. PMID: 1754955.
Article12. Strasberg SM, Brunt LM. 2010; Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 211:132–138. DOI: 10.1016/j.jamcollsurg.2010.02.053. PMID: 20610259.
Article13. Wright KD, Wellwood JM. 1998; Bile duct injury during laparoscopic cholecystectomy without operative cholangiography. Br J Surg. 85:191–194. DOI: 10.1046/j.1365-2168.1998.00568.x. PMID: 9501813.
Article14. Bismuth H, Majno PE. 2001; Biliary strictures: classification based on the principles of surgical treatment. World J Surg. 25:1241–1244. DOI: 10.1007/s00268-001-0102-8. PMID: 11596882.
Article15. Strasberg SM, Hertl M, Soper NJ. 1995; An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 180:101–125. PMID: 8000648.16. Lillemoe KD, Petrofski JA, Choti MA, Venbrux AC, Cameron JL. 2000; Isolated right segmental hepatic duct injury: a diagnostic and therapeutic challenge. J Gastrointest Surg. 4:168–177. DOI: 10.1016/S1091-255X(00)80053-0. PMID: 10675240.
Article17. Kaffes AJ, Hourigan L, De Luca N, Byth K, Williams SJ, Bourke MJ. 2005; Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc. 61:269–275. DOI: 10.1016/S0016-5107(04)02468-X. PMID: 15729238.
Article18. Perini RF, Uflacker R, Cunningham JT, Selby JB, Adams D. 2005; Isolated right segmental hepatic duct injury following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 28:185–195. DOI: 10.1007/s00270-004-2678-5. PMID: 15770390.
Article19. Perera MT, Monaco A, Silva MA, Bramhall SR, Mayer AD, Buckels JA, et al. 2011; Laparoscopic posterior sectoral bile duct injury: the emerging role of nonoperative management with improved long-term results after delayed diagnosis. Surg Endosc. 25:2684–2691. DOI: 10.1007/s00464-011-1630-4. PMID: 21416174.
Article20. LeBedis CA, Bates DDB, Soto JA. 2017; Iatrogenic, blunt, and penetrating trauma to the biliary tract. Abdom Radiol (NY). 42:28–45. DOI: 10.1007/s00261-016-0856-y. PMID: 27503381.
Article21. Bujanda L, Calvo MM, Cabriada JL, Orive V, Capelastegui A. 2003; MRCP in the diagnosis of iatrogenic bile duct injury. NMR Biomed. 16:475–478. DOI: 10.1002/nbm.853. PMID: 14696004.
Article22. Palmucci S, Roccasalva F, Piccoli M, Fuccio Sanzà G, Foti PV, Ragozzino A, et al. 2017; Contrast-enhanced magnetic resonance cholangiography: practical tips and clinical indications for biliary disease management. Gastroenterol Res Pract. 2017:2403012. DOI: 10.1155/2017/2403012. PMID: 28348578. PMCID: PMC5350537.
Article23. Li J, Frilling A, Nadalin S, Radunz S, Treckmann J, Lang H, et al. 2010; Surgical management of segmental and sectoral bile duct injury after laparoscopic cholecystectomy: a challenging situation. J Gastrointest Surg. 14:344–351. DOI: 10.1007/s11605-009-1087-0. PMID: 19911237.
Article24. Schipper IB, Rauws EA, Gouma DJ, Obertop H. 1996; Diagnosis of right hepatic duct injury after cholecystectomy: the use of cholangiography through percutaneous drainage catheters. Gastrointest Endosc. 44:350–354. DOI: 10.1016/S0016-5107(96)70181-5. PMID: 8885363.
Article25. Meyers WC, Peterseim DS, Pappas TN, Schauer PR, Eubanks S, Murray E, et al. 1996; Low insertion of hepatic segmental duct VII-VIII is an important cause of major biliary injury or misdiagnosis. Am J Surg. 171:187–191. DOI: 10.1016/S0002-9610(99)80097-X. PMID: 8554138.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful non-surgical treatment for isolated right anterior section bile duct injury following laparoscopic cholecystectomy: Report of a case
- Acetic acid sclerotherapy for treatment of biliary leak from an isolated right posterior sectoral duct after cholecystectomy
- Relationship between the risk of bile duct injury during laparoscopic cholecystectomy and the types of preoperative magnetic resonance cholangiopancreatiocography (MRCP)
- Recent classifications of the common bile duct injury
- Importance of critical view of safety in laparoscopic cholecystectomy: a survey of 120 serial patients, with no incidence of complications