J Korean Orthop Assoc.
2012 Jun;47(3):171-177. 10.4055/jkoa.2012.47.3.171.
The Effectiveness of C-Reactive Protein Surveillance as a Method to Monitor the Post-Operative Antibiotics Administration after Total Knee Replacement Arthroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Hanyang University, Seoul, Korea. chhchoi@hanyang.ac.kr
- KMID: 2106644
- DOI: http://doi.org/10.4055/jkoa.2012.47.3.171
Abstract
- PURPOSE
To evaluate the effectiveness of using C-reactive protein (CRP) surveillance as a method to monitor the effect of postoperative antibiotics for the prevention of early infection after total knee replacement arthroplasty (TKRA).
MATERIALS AND METHODS
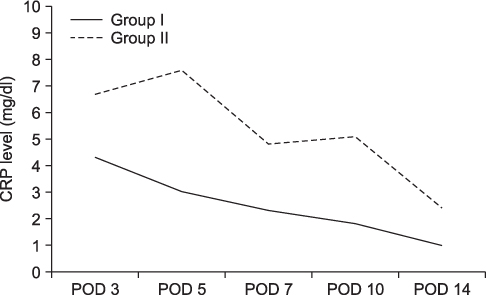
A prospective study was performed in 115 primary TKRAs. We examined the values of CRP of all cases on the 3rd, 5th, 7th, 10th and 14th days post-operatively. Some patients were administrated additional antibiotics under certain specific situations based on the pattern of CRP. The patients were divided into two groups: group I with planned period of administration and group II with administration longer than the planned period.
RESULTS
No acute infection after TKRA due to CRP surveillance was observed. The mean duration of antibiotics administration was 5.9 days in all cases, 5 days in group I and 13.3 days in group II. Twelve cases (10.4%) were included in group II. The CRP was increased on the 5th and 10th days after operation in group II.
CONCLUSION
The surveillance of CRP was thought to be helpful in monitoring the effects of post-operative antibiotics and prevention of early infection after TKRA.
MeSH Terms
Figure
Reference
-
1. Bryan CS, Morgan SL, Caton RJ, Lunceford EM Jr. Cefazolin versus cefamandole for prophylaxis during total joint arthroplasty. Clin Orthop Relat Res. 1988. (228):117–122.
Article2. Meehan J, Jamali AA, Nguyen H. Prophylactic antibiotics in hip and knee arthroplasty. J Bone Joint Surg Am. 2009. 91:2480–2490.
Article3. White J, Kelly M, Dunsmuir R. C-reactive protein level aft er total hip and total knee replacement. J Bone Joint Surg Br. 1998. 80:909–911.4. Chung HK, Choi CH, Shon JH. A study for the change of C-reactive protein aft er the total knee replacement. J Korean Knee Soc. 1996. 8:74–80.5. Curtis M, Graves N, Birrell F, et al. A comparison of competing methods for the detection of surgical-site infections in patients undergoing total arthroplasty of the knee, partial and total arthroplasty of hip and femoral or similar vascular bypass. J Hosp Infect. 2004. 57:189–193.
Article6. Debarge R, Nicolle MC, Pinaroli A, Ait Si Selmi T, Neyret P. Surgical site infection aft er total knee arthroplasty: a monocenter analysis of 923 first-intention implantations. Rev Chir Orthop Reparatrice Appar Mot. 2007. 93:582–587.7. Pfitzner T, Krocker D, Perka C, Matziolis G. C-reactive protein. An independent risk factor for the development of infection aft er primary arthroplasty. Orthopade. 2008. 37:1116–1120.8. Tsukayama DT, Goldberg VM, Kyle R. Diagnosis and management of infection aft er total knee arthroplasty. J Bone Joint Surg Am. 2003. 85-A:Suppl 1. S75–S80.9. Bottner F, Wegner A, Winkelmann W, Becker K, Erren M, Götze C. Interleukin-6, procalcitonin and TNF-alpha: markers of peri-prosthetic infection following total joint replacement. J Bone Joint Surg Br. 2007. 89:94–99.10. Monneret G, Doche C, Durand DV, Lepape A, Bienvenu J. Procalcitonin as a specific marker of bacterial infection in adults. Clin Chem Lab Med. 1998. 36:67–68.
Article11. Bilgen O, Atici T, Durak K, Karaeminoğullari O, Bilgen MS. C-reactive protein values and erythrocyte sedimentation rates aft er total hip and total knee arthroplasty. J Int Med Res. 2001. 29:7–12.12. Dupont C, Rodenbach J, Flachaire E. The value of C-reactive protein for postoperative monitoring of lower limb arthroplasty. Ann Readapt Med Phys. 2008. 51:348–357.
Article13. Larsson S, Thelander U, Friberg S. C-reactive protein (CRP) levels aft er elective orthopedic surgery. Clin Orthop Relat Res. 1992. (275):237–242.14. Tillett WS, Francis T. Serological reactions in pneumonia with a non-protein somatic fraction of pneumococcus. J Exp Med. 1930. 52:561–571.
Article15. Choi CH, Choi JW, Sung IH, Song JC. Early change of C-reactive protein level in TKA: antibiotic-loaded vs plain bone cement. J Korean Knee Soc. 2006. 18:80–85.16. Shih LY, Wu JJ, Yang DJ. Erythrocyte sedimentation rate and C-reactive protein values in patients with total hip arthroplasty. Clin Orthop Relat Res. 1987. (225):238–246.
Article17. Park KK, Kim TK, Chang CB, Yoon SW, Park KU. Normative temporal values of CRP and ESR in unilateral and staged bilateral TKA. Clin Orthop Relat Res. 2008. 466:179–188.
Article18. Pepys MB. C-reactive protein and the acute phase response. Nature. 1982. 296:12.
Article19. Holt BT, Parks NL, Engh GA, Lawrence JM. Comparison of closed-suction drainage and no drainage aft er primary total knee arthroplasty. Orthopedics. 1997. 20:1121–1124.20. Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total knee arthroplasties. Clin Orthop Relat Res. 1998. 347:188–193.
Article21. Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE. Factors associated with prolonged wound drainage aft er primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007. 89:33–38.22. Elek SD. Experimental staphylococcal infections in the skin of man. Ann N Y Acad Sci. 1956. 65:85–90.
Article23. Padovani P. Surgical infection in orthopedic surgery. Preparation of patients and postoperative care. Rev Chir Orthop Reparatrice Appar Mot. 1969. 55:201–207.24. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961. 50:161–168.25. Polk HC Jr, Lopez-Mayor JF. Postoperative wound infection: a prospective study of determinant factors and prevention. Surgery. 1969. 66:97–103.26. Boyd RJ, Burke JF, Colton T. A double-blind clinical trial of prophylactic antibiotics in hip fractures. J Bone Joint Surg Am. 1973. 55:1251–1258.
Article27. Fogelberg EV, Zitzmann EK, Stinchfield FE. Prophylactic penicillin in orthopaedic surgery. J Bone Joint Surg Am. 1970. 52:95–98.
Article28. Muirhead AG, Campbell A. Prophylactic antibiotic in knee arthroplasty. J Bone Joint Surg Br. 1993. 75:667.
Article29. Pavel A, Smith RL, Ballard A, Larsen IJ. Prophylactic antibiotics in clean orthopaedic surgery. J Bone Joint Surg Am. 1974. 56:777–782.
Article30. Vainionpää S, Wilppula E, Lalla M, Renkonen OV, Rokkanen P. Cefamandole and isoxazolyl penicillins in antibiotic prophylaxis of patients undergoing total hip or knee-joint arthroplasty. Arch Orthop Trauma Surg. 1988. 107:228–230.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Geometric Total Knee Arthroplasty: A Case Report
- Osteotomy of the Tibial Tubercle in difficult Total Knee Arthroplasty
- Staged Reimplantation Using Cement Spacer Containing Antibiotics in Infected Total Knee Arthroplasty
- Two-stage revision of infected total knee arthroplasty
- Synovial Impingement after Total Knee Replacement Arthroplasty: A Case Report