J Korean Orthop Assoc.
2008 Feb;43(1):101-106. 10.4055/jkoa.2008.43.1.101.
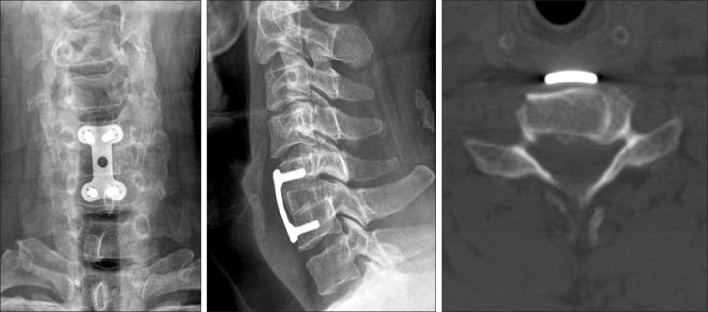
Effectiveness of the New Modified Smith-Robinson Bone Graft for Cervical Anterior Interbody Fusion
- Affiliations
-
- 1Department of Orthopaedic Surgery, School of Medicine, Gyeongsang National University, Jinju, Korea. ssurgeon@nongae.gsnu.ac.kr
- KMID: 2106423
- DOI: http://doi.org/10.4055/jkoa.2008.43.1.101
Abstract
-
PURPOSE: We attempted to evaluate the effectiveness of the new modified Smith-Robinson bone graft method for performing cervical anterior interbody fusion.
MATERIALS AND METHODS
Forty-two patients had anterior interbody fusion on the cervical spine, using an anterior approach and the new modified Smith-Robinson's method (NMSR), between September 2001 and June 2006. There were 30 males and 12 females, with an average age of 51.2 years and the mean follow up period was 39.5 months. We measured the area from C4 to C6 in 32 cases. This was compared with the contact area of the bone graft of the NMSR method and the Original Smith-Robinson method (OSR). We also checked the time to bone union and changes of Cobb's angle at the final follow-up to evaluate the effectiveness of the NMSR.
RESULTS
Bony fusion was obtained in all cases. The average size of the OSR were 169 and 152 mm2, in the males and females respectively, whereas those of the NMSR were 263, and 228 mm2. Therefore, the average size of the NMSR increased to 94 mm2 and 76 mm2 than those of the OSR method in the males and females. The average time to radiological bone union was 9.6 weeks and the changes of Cobb's angle at final follow-up were 2.5+/-2.6degrees.
CONCLUSION
The NMSR technique was a very effective method for cervical anterior interbody fusion. It could enlarge the bone graft size about 50-56% compared with the OSR technique. It also shortened the period of bone union and also increased the bone union rate.
Keyword
Figure
Cited by 1 articles
-
Usefulness of Anterior Cervical Interbody Fusion Using Locally Harvested Bone: Minimum 5-Year Follow-Up
Dae Moo Shim, Tae Kyun Kim, Sung Kyun Oh, Seung Whan Kuk, Bong Jun Jang, Ji Woong Choi
J Korean Orthop Assoc. 2016;51(3):191-198. doi: 10.4055/jkoa.2016.51.3.191.
Reference
-
1. An HS, Simpson JM, Glover JM, Stephan J. Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion. A prospective multicenter study. Spine. 1995. 20:2211–2216.2. Bailey RW, Badgley CE. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am. 1960. 42:565–594.
Article3. Böhler J, Gaudernak T. Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma. 1980. 20:203–205.4. Bolesta MJ, Rechtine GR 2nd, Chrin AM. One- and two-level anterior cervical discectomy and fusion: the effect of plate fixation. Spine J. 2002. 2:197–203.
Article5. Brantigan JW. Pseudarthrosis rate after allograft posterior lumbar interbody fusion with pedicle screw and plate fixation. Spine. 1994. 19:1271–1279.
Article6. Brodke DS, Zdeblick TA. Modified Smith-Robinson procedure for anterior cervical discectomy and fusion. Spine. 1992. 17:Suppl 10. S427–S430.
Article7. Cloward RB. Treatment of acute fractures and fracture-dislocations of the cervical spine by vertebral-body fusion. A report of eleven cases. J Neurosurg. 1961. 18:201–209.8. Ebraheim NA, Fow J, Xu R, Yeasting RA. The vertebral body depths of the cervical spine and its relation to anterior plate-screw fixation. Spine. 1998. 23:2299–2302.
Article9. Jenis LG, An HS, Simpson JM. A prospective comparison of the standard and reverse robinson cervical grafting techniques: radiographic and clinical analyses. J Spinal Disord. 2000. 13:369–373.
Article10. Kumaresan S, Yoganandan N, Pintar FA. Finite element analysis of anterior cervical spine interbody fusion. Biomed Mater Eng. 1997. 7:221–230.
Article11. Lee JK, Ahn JS, Kim SB, Hong CH, Lee JB. Influence of plate position on fusion time and clinical outcomes after anterior cervical interbody fusion. J Korean Soc Spine Surg. 2005. 12:22–27.
Article12. Park HJ, Rah JH, Yoon YS. Anterior cervical fusion with cervical spine locking plate system. J Korean Orthop Assoc. 1996. 31:52–58.
Article13. Robinson RA, Smith GW. Anterolateral cervical disk removing and interbody fusion for cervical disk syndrome. Bull John Hopkins Hospital. 1955. 96:223–224.14. Song KJ, Choi BR, Yang KH, Lee KB. Results of one level anterior cervical discectomy and fusion in the degenerative cervical spinal disorder. J Korean Orthop Assoc. 2003. 38:282–288.15. Song KJ, Lee KB, Kim SR. Availability of anterior cervical plating according to the severity of injury in distractive flexion injury in lower cervical spine. J Korean Orthop Assoc. 2005. 40:195–202.
Article16. Suchomel P, Barsa P, Buchvald P, Svobodnik A, Vanickova E. Autologous versus allogenic bone grafts in instrumented anterior cervical discectomy and fusion: a prospective study with respect to bone union pattern. Eur Spine J. 2004. 13:510–515.
Article17. Wang JC, McDonough PW, Endow K, Kanim LE, Delamarter RB. The effect of cervical plating on single-level anterior cervical discectomy and fusion. J Spinal Disord. 1999. 12:467–471.
Article18. Young WF, Rosenwasser RH. An early comparative analysis of the use of fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine. 1993. 18:1123–1124.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Analysis of Treatment of Cervical Fracture and Dislocation
- Analysis of Noninstrumented Anterior Cervical Discectomy and Interbody Fusion in Degenerative Cervical Disease
- A Bone Graft Anchoring with Wire in Cervical Anterior Interbody Fusion(Technical Note)
- Clinical Analysis of Surgery Treatment in Cervical Disc Disease: Long-Term Follow Up
- The Availability of Autogenous Bicortical Iliac Bone Graft in Anterior Cervical Interbody Fusion