J Korean Orthop Assoc.
2007 Feb;42(1):136-140. 10.4055/jkoa.2007.42.1.136.
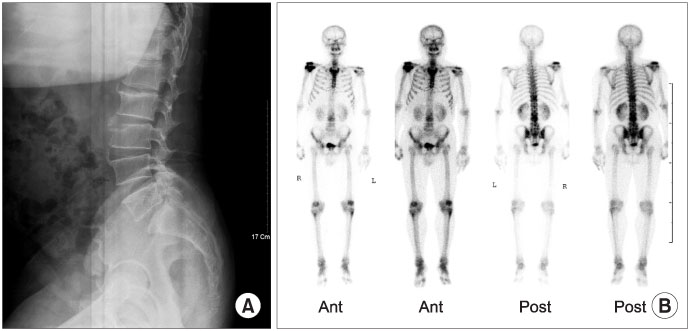
Clinical Findings of Brucellar Spondylitis: A Case Report
- Affiliations
-
- 1Department of Orthopaedics Surgery, Wonkwang University Hospital, Iksan, Korea.
- 2Department of Orthopaedics Surgery, Gunsan Medical Center of Wonkwang University Hospital, Gunsan, Korea. ospjy1222@empas.com
- KMID: 2106387
- DOI: http://doi.org/10.4055/jkoa.2007.42.1.136
Abstract
- Brucellosis is an endemic zoonotic disease that it is rare in Korea. However, there have been regional increases in its prevalence. Brucellar spondylitis is difficult to diagnose because the clinical presentation is often variable and nonspecific. Therefore, it is often overlooked in a differential diagnosis of back pain. A culture and microbiologic study is the choice for diagnosing brucellar spondylitis. If treatment is not properly done, brucellar spondylitis can result in severe complications including neurobrucellosis. Medical treatments for brucellar spondylitis are generally encouraged, even though surgical treatments are performed in cases showing spinal instability caused by progressive spinal cord and root compression. The combination of doxycycline and streptomycin for 3 weeks followed by a combination of doxycycline and rifampicin for 6 months is the most effective regimen. We report a case of brucellar spondylitis to highlight it as one of the possible cause of back pain in Korea.
Keyword
MeSH Terms
Figure
Reference
-
1. Colmenero JD, Reguera JM, Fernandez-Nebro A, Cabrera-Franguelo F. Osteoarticular complications of brucellosis. Ann Rheum Dis. 1991. 50:23–26.
Article2. Geyik MF, Gur A, Nas K. Musculoskeletal involvement of brucellosis in different age groups: a study of 195 cases. Swiss Med Wkly. 2002. 132:98–105.3. Lulu AR, Araj GF, Khateeb MI, Mustafa MY, Yusuf AR, Fenech FF. Human brucellosis in Kuwait: a prospective study of 400 cases. Q J Med. 1988. 66:39–54.4. Madkour MM, Kasper E, Hauser DL. Brucellosis. 2001. 2:14th ed. McGraw-Hill Professional;969–971.5. Ozaksoy D, Yucesoy K, Yucesoy M, Kovanlikaya I, Yuce A, Naderi S. Brucellar spondylitis: MRI findings. Eur Spine J. 2001. 10:529–533.
Article6. Reitman CA, Watters WC 3rd. Spinal brucellosis: case report in the United States. Spine. 2002. 27:E250–E252.7. Sharif HS, Aideyan OA, Clark DC. Brucellar and tuberculous spondylitis: comparative imaging features. Radiology. 1989. 171:419–425.
Article8. Solera J, Martinez-Alfraro E, Espinosa A. Recognition and optimum treatment of brucellosis. Drug. 1997. 53:245–256.
Article9. Whee SM, Eoh W, Nam DH. Clinical evaluation of surgical treatments for ten cases of tuberculous spondylitis. J Korean Neurosurg Soc. 2001. 30:1314–1319.