J Korean Surg Soc.
2011 Aug;81(2):141-145. 10.4174/jkss.2011.81.2.141.
Cystic lymphangioma of the pancreas
- Affiliations
-
- 1Department of Surgery, Catholic University of Daegu School of Medicine, Daegu, Korea. bilgekar@yahoo.com
- 2Department of Pathology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 2096669
- DOI: http://doi.org/10.4174/jkss.2011.81.2.141
Abstract
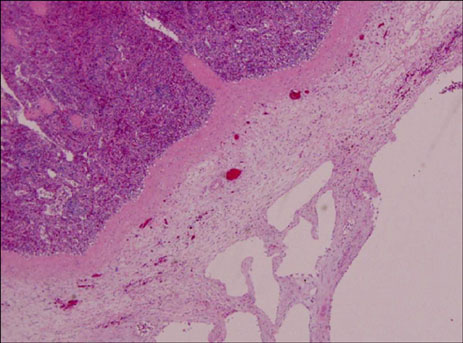
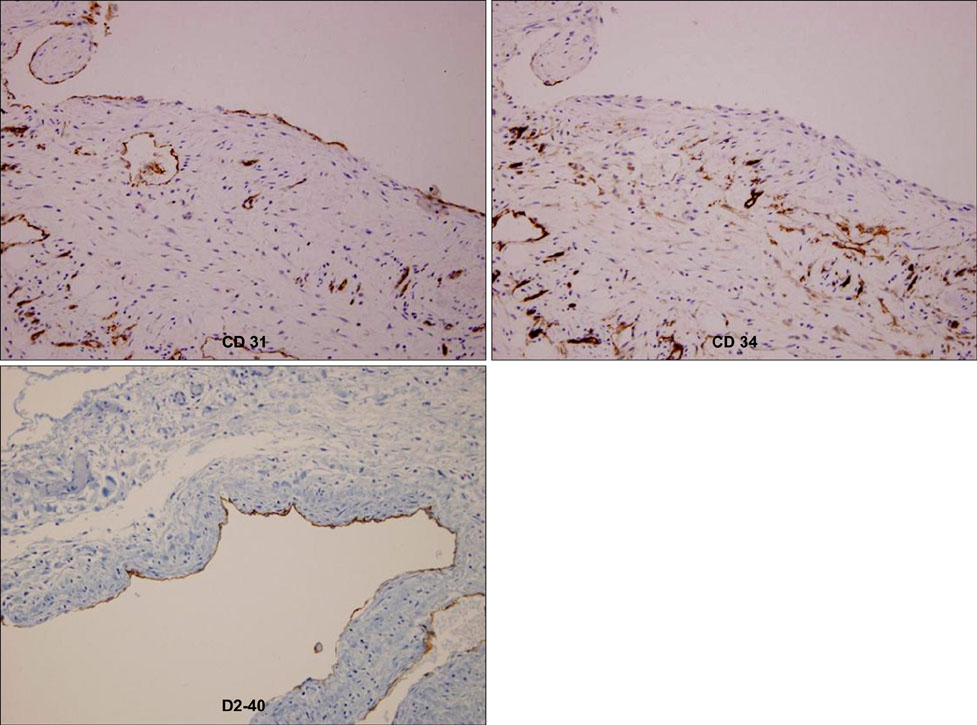
- Lymphangioma is a benign form of neoplasm arising from the lymphatic system. It occurs as a result of congenital malformations of the lymphatics leading to the obstruction of local lymph flow and the development of lymphangiectasia. Lymphangiomas are common in pediatric patients, in the soft tissues of the neck and the axillae, but lymphangioma of the pancreas is extremely rare, accounting for less than 1% of these tumors. It occurs more frequently in females and is often located in the distal pancreas. Although extremely rare, cystic lymphangioma of the pancreas should be taken into consideration as a differential diagnosis of pancreatic cystic or retroperitoneal lesions, especially in women. Herein, we report on a case of cystic lymphangioma of the distal pancreas in a 37-year-old woman who was treated with complete surgical resection with a review of the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Losanoff JE, Richman BW, El-Sherif A, Rider KD, Jones JW. Mesenteric cystic lymphangioma. J Am Coll Surg. 2003. 196:598–603.2. Leung TK, Lee CM, Shen LK, Chen YY. Differential diagnosis of cystic lymphangioma of the pancreas based on imaging features. J Formos Med Assoc. 2006. 105:512–517.3. Colovic RB, Grubor NM, Micev MT, Atkinson HD, Rankovic VI, Jagodic MM. Cystic lymphangioma of the pancreas. World J Gastroenterol. 2008. 14:6873–6875.4. Paal E, Thompson LD, Heffess CS. A clinicopathologic and immunohistochemical study of ten pancreatic lymphangiomas and a review of the literature. Cancer. 1998. 82:2150–2158.5. Schneider G, Seidel R, Altmeyer K, Remberger K, Pistorius G, Kramann B, et al. Lymphangioma of the pancreas and the duodenal wall: MR imaging findings. Eur Radiol. 2001. 11:2232–2235.6. Bonhomme A, Broeders A, Oyen RH, Stas M, De Wever I, Baert AL. Cystic lymphangioma of the retroperitoneum. Clin Radiol. 2001. 56:156–158.7. Iwabuchi A, Otaka M, Okuyama A, Jin M, Otani S, Itoh S, et al. Disseminated intra-abdominal cystic lymphangiomatosis with severe intestinal bleeding: a case report. J Clin Gastroenterol. 1997. 25:383–386.8. Steyaert H, Guitard J, Moscovici J, Juricic M, Vaysse P, Juskiewenski S. Abdominal cystic lymphangioma in children: benign lesions that can have a proliferative course. J Pediatr Surg. 1996. 31:677–680.9. Kalof AN, Cooper K. D2-40 immunohistochemistry: so far! Adv Anat Pathol. 2009. 16:62–64.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cystic lymphangioma of the pancreas: a case report
- Cystic Lymphangioma of the Pancreas
- Cystic lymphangioma of the pancreas: A Case Report
- Cystic lymphangioma of the pancreas mimicking pancreatic pseudocyst
- Retroperitoneal Cystic Lymphangioma Diagnosed by Endoscopic Ultrasound-Guided Fine Needle Aspiration