J Korean Surg Soc.
2011 Aug;81(2):75-84. 10.4174/jkss.2011.81.2.75.
Review of atypical cytology of thyroid nodule according to the Bethesda system and its beneficial effect in the surgical treatment of papillary carcinoma
- Affiliations
-
- 1Department of Surgery, Gachon University Gil Hospital, Gachon University of Medicine and Science, Incheon, Korea.
- 2Department of Hospital Pathology, St. Vincent Hospital, The Catholic University of Korea School of Medicine, Suwon, Korea. ppgg2@catholic.ac.kr
- 3Department of Surgery, St. Vincent Hospital, The Catholic University of Korea School of Medicine, Suwon, Korea.
- KMID: 2096660
- DOI: http://doi.org/10.4174/jkss.2011.81.2.75
Abstract
- PURPOSE
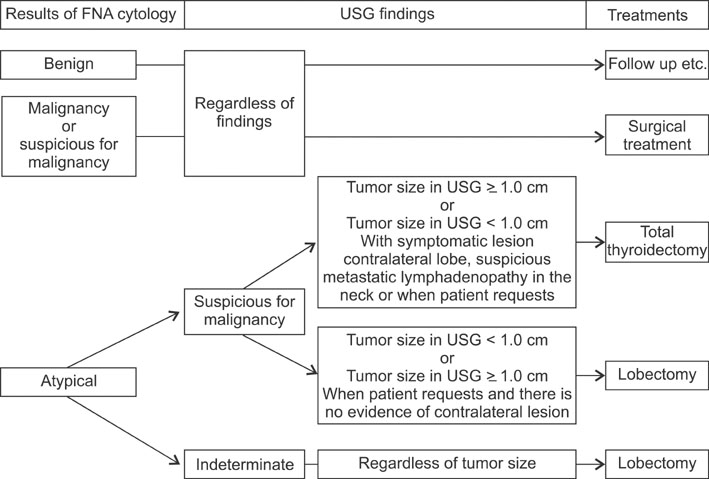
For the atypical cases of fine needle aspiration (FNA) cytology of thyroid nodules, ultrasonographic findings are a primary guideline for the surgical treatment. However, they have the intrinsic risk of overtreatment, as well. In this study we examined whether the Bethesda system could provide a real effect on the diagnostic rate of atypical cytology, and thereby reduce the number of cases diagnosed as atypical from FNA cytology.
METHODS
We reviewed 166 cases diagnosed as atypical by FNA cytology at this institute between the years 2005 to 2010. We classified these cases on the basis of ultrasonographic and cytological findings and compared them with the histological results.
RESULTS
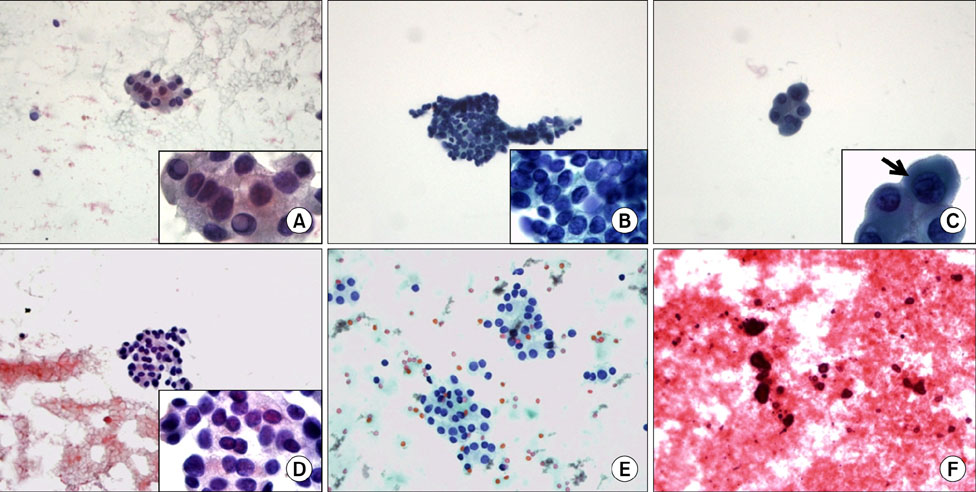
Ultrasonographically, findings suspicious for malignancy and indeterminate were associated with 83.7% and 47.2% of malignancy rates, respectively. Cytopathologically, the malignancy rates varied according to the main cytological features and the highest malignancy rate was 77.3%. Based on the Bethesda system, 39.2% of the cases diagnosed as atypical could be grouped into the category of suspicious for malignancy and yielded a malignancy rate of 76.9%.
CONCLUSION
Although ultrasonography provides an excellent guideline for the surgical treatment of atypical cases, it also showed considerable risk of overtreatment. The Bethesda system did not offer definitive effects on the rate of atypical cytology, but this system seemed to provide stricter boundaries for the atypical cytology and to aid in reducing the rates thereof. This in turn may permit that more limited cases are allotted to ultrasonographic decision making.
Keyword
Figure
Reference
-
1. American Thyroid Association (ATA) Guidelines Task-force on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.2. Tan WJ, Sanghvi K, Liau KH, Low CH. An audit study of the sensitivity and specificity of ultrasound, fine needle aspiration cytology and frozen section in the evaluation of thyroid malignancies in a tertiary institution. Ann Acad Med Singapore. 2010. 39:359–362.3. Marhefka GD, McDivitt JD, Shakir KM, Drake AJ 3rd. Diagnosis of follicular neoplasm in thyroid nodules by fine needle aspiration cytology: does the result, benign vs. suspicious for a malignant process, in these nodules make a difference? Acta Cytol. 2009. 53:517–523.4. Sherman JF, Leiman G, Naud S, Nathan MH, Ambaye AB. Follicular and Hürthle cell lesions of the thyroid: can inconclusive results be minimized? Acta Cytol. 2008. 52:659–664.5. Faquin WC. The thyroid gland: recurring problems in histologic and cytologic evaluation. Arch Pathol Lab Med. 2008. 132:622–632.6. Cibas ES, Ali SZ. The Bethesda system for reporting thyroid cytopathology: definitions, criteria, and explanatory notes. 2010. New York: Springer.7. Cibas ES, Ali SZ. The bethesda system for reporting thyroid cytopathology. Thyroid. 2009. 19:1159–1165.8. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation: multicenter retrospective study. Radiology. 2008. 247:762–770.9. Theoharis CG, Schofield KM, Hammers L, Udelsman R, Chhieng DC. The Bethesda thyroid fine-needle aspiration classification system: year 1 at an academic institution. Thyroid. 2009. 19:1215–1223.10. Sorrenti S, Trimboli P, Catania A, Ulisse S, De Antoni E, D'Armiento M. Comparison of malignancy rate in thyroid nodules with cytology of indeterminate follicular or indeterminate Hurthle cell neoplasm. Thyroid. 2009. 19:355–360.11. Ginat DT, Butani D, Giampoli EJ, Patel N, Dogra V. Pearls and pitfalls of thyroid nodule sonography and fine-needle aspiration. Ultrasound Q. 2010. 26:171–178.12. Cibas ES. Fine-needle aspiration in the work-up of thyroid nodules. Otolaryngol Clin North Am. 2010. 43:257–271. vii–viii.13. Rabaglia JL, Kabbani W, Wallace L, Holt S, Watumull L, Pruitt J, et al. Effect of the Bethesda system for reporting thyroid cytopathology on thyroidectomy rates and malignancy risk in cytologically indeterminate lesions. Surgery. 2010. 148:1267–1272.14. Kwak JY, Kim EK, Kim MJ, Hong SW, Choi SH, Son EJ, et al. The role of ultrasound in thyroid nodules with a cytology reading of "suspicious for papillary thyroid carcinoma". Thyroid. 2008. 18:517–522.15. Piana S, Frasoldati A, Ferrari M, Valcavi R, Froio E, Barbieri V, et al. Is a five-category reporting scheme for thyroid fine needle aspiration cytology accurate? Experience of over 18 000 FNAs reported at the same institution during 1998-2007. Cytopathology. 2011. 22:164–173.16. Ardito G, Rossi ED, Revelli L, Moschella F, Giustozzi E, Fadda G, et al. The role of fine-needle aspiration performed with liquid-based cytology in the surgical management of thyroid lesions. In Vivo. 2010. 24:333–337.17. Schinstine M. A brief description of the Bethesda System for reporting thyroid fine needle aspirates. Hawaii Med J. 2010. 69:176–178.18. Crippa S, Mazzucchelli L, Cibas ES, Ali SZ. The Bethesda system for reporting thyroid fine-needle aspiration specimens. Am J Clin Pathol. 2010. 134:343–344.19. Pang T, Ihre-Lundgren C, Gill A, McMullen T, Sywak M, Sidhu S, et al. Correlation between indeterminate aspiration cytology and final histopathology of thyroid neoplasms. Surgery. 2010. 148:532–537.20. Keskek M, Ocak S, Ozalp N, Koc M, Tez M. Clinical significance of Hürthle cells in fine needle aspiration biopsy for multinodular goitre. Endocr Regul. 2010. 44:65–68.21. Jo VY, Stelow EB, Dustin SM, Hanley KZ. Malignancy risk for fine-needle aspiration of thyroid lesions according to the Bethesda System for Reporting Thyroid Cytopathology. Am J Clin Pathol. 2010. 134:450–456.22. Lee K, Jung CK, Lee KY, Bae JS, Lim DJ, Jung SL. Application of bethesda system for reporting thyroid aspiration cytology. Korean J Pathol. 2010. 44:521–527.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- Thyroid nodules with Bethesda System IV Cytology: Can Ultrasonography Differentiate Malignancy from Benign?
- Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- Associations between Bethesda categories and tumor characteristics of conventional papillary thyroid carcinoma
- Ultrasonographic imaging of papillary thyroid carcinoma variants