Korean Circ J.
2007 Sep;37(9):419-424. 10.4070/kcj.2007.37.9.419.
Lesion Location: Its Impacts on the Procedural and Postprocedural Outcomes of Unprotected Left Main Coronary Stenting
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, College of Medicine, Yeungnam University, Daegu, Korea. yjkim@med.yu.ac.kr
- 2Department of Internal Medicine, College of Medicine, Keimyung University, Dongsan Hospital, Daegu, Korea.
- 3Department of Internal Medicine, College of Medicne, Inje University, Busan Baik Hospital, Busan, Korea.
- KMID: 2093978
- DOI: http://doi.org/10.4070/kcj.2007.37.9.419
Abstract
-
BACKGROUND AND OBJECTIVES: Percutaneous coronary intervention (PCI) for unprotected left main coronary artery (LMCA) stenosis is a promising technique in the drug-eluting stent era. However, there is a lack of data as to the impact of the lesion location in the LMCA on the procedural and postprocedural outcomes. The aim of this study is to evaluate the effect of lesion location on the procedural and postprocedural outcomes.
SUBJECTS AND METHODS
From July 2003 to January 2006, we enrolled 82 patients (Males: n=49), who underwent PCI for unprotected LMCA stenosis at Yeungnam University Medical Center, Keimyung University Dong-san Hospital and In-je University Baik Hospital in Busan. The patients were divided into two groups according to the lesion location. Group 1 (n=38) was defined as those patients who had a significant stenosis in the ostium and/or body. Group 2 (n=44) was defined as those patients had a left main coronary lesion involving a bifurcation. All the patients had a sirolimus eluting stent (Cypher, Cordis) deployed into the LMCA stenosis. Stenting techniques such as the T, crush and kissing stent techniques for treating the LMCA were used at the discretion of the operator and according to the characteristics of the lesion location. The in-hospital outcomes were compared between the two groups and follow-up coronary angiography was performed after 6 months; the major adverse cardiac events (MACE) and restenosis were analyzed between the two groups.
RESULTS
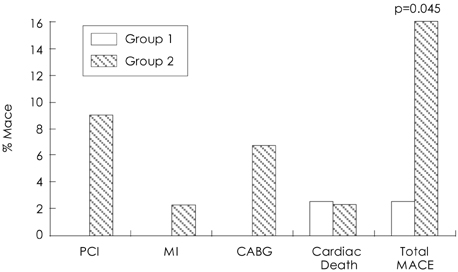
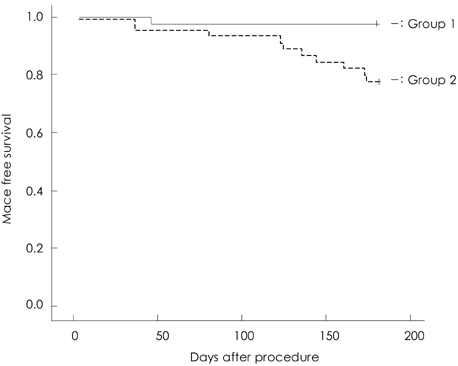
The baseline characteristics between the two groups were not statistically different. The procedural outcomes showed that for the stenting methods, the conventional stent technique was the only one used in all cases of Group 1, but the kissing, T stenting and Crush techniques were also used in Group 2 (p=0.001). The clinical outcomes showed that that there was no statistical difference for the in-hospital MACEs between the two groups, but for the out-of hospital MACEs at 6 month, the target lesion revascularizatin rates, including PCI or bypass graft operation, in Group 1 were higher than those in Group 2 (0% vs 13.6%, respectively p=0.043). Both groups had one cardiac death each (2.3% vs 2.6% respectively) and there was 1 MACE in Group 1 and 7 MACEs in Group 2 (2.6% vs 16%, respectively, p=0.045). The angiographic outcomes at 6 month showed that all 8 significant restenosis cases were included in Group 2 (18%, 9.7% in the total population); the restenosis site was the left circumflex artery in all cases.
CONCLUSION
PCI with using drug eluting stents in the left main lesion showed favorable short term outcomes in selected patients. The lesion location is also an important factor for the clinical and angiographical outcomes.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Novel Coronary Stent Platforms
Bon-Kwon Koo, Peter J. Fitzgerald
Korean Circ J. 2008;38(8):393-397. doi: 10.4070/kcj.2008.38.8.393.
Reference
-
1. Caracciolo EA, Davis KB, Sopko G, et al. Comparison of surgical and medical group survival in patients with left main coronary artery disease. Circulation. 1995. 91:2325–2334.2. Takaro T, Peduzzi P, Detre KM, et al. Survival in subgroups of patients with left main coronary artery disease. Circulation. 1982. 66:14–22.3. Smith SC, Dove JT, Jacobs AK, et al. ACC/AHA guidelines of percutaneous coronary intervention (revision of 1993 PTCA guidelines) executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2001. 37:2215–2239.4. Silber S, Albertsson P, Marco J, et al. Guidelines for percutaneous coronary intervention. Eur Heart J. 2005. 26:804–847.5. Tan WA, Tamai H, Park SJ, et al. Long-term clinical outcomes after unprotected left main trunk percutaneous revascularization in 279 patients. Circulation. 2001. 104:1609–1614.6. Morice MC, Serruys PW, Sousa JE, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002. 346:1773–1780.7. Degertekin M, Serruys PW, Foley DP, et al. Persistent inhibition of neointimal hyperplasia after sirolimus-eluting stent implantation: long-term (up to 2 years) clinical, angiographic, and intravascular ultrasound follow-up. Circulation. 2002. 106:1610–1613.8. Lenzen MJ, Boersma E, Bertrand ME, et al. Management and outcome of patients with established coronary artery disease. Eur Heart J. 2005. 26:1169–1179.9. Ellis SG, Tamai H, Nobuyoshi M, et al. Contemporary percutaneous treatment of unprotected left main coronary stenoses: initial results from a multicenter registry analysis 1994-1996. Circulation. 1997. 96:3867–3872.10. DeMots H, Rosch J, McAnulty JH, Rahimtoola SH. Left main coronary artery disease. Cardiovasc Clin. 1977. 8:201–211.11. Topaz O, Warner M, Lanter P, et al. Isolated significant left main coronary artery stenosis: angiographic, hemodynamic and clinical findings in 16 patients. Am Heart J. 1991. 122:1308–1314.12. Miller GA, Honey M, el-Sayed H. Isolated coronary ostial stenosis. Cathet Cardiovasc Diagn. 1986. 12:30–34.13. Park SJ, Park SW, Hong MK, et al. Stenting of unprotected left main coronary artery stenosis without anticoagulation: immediate and late outcomes. Korean Circ J. 1997. 27:947–957.14. Park JH, Cho YH, Lee SH, et al. Long term clinical follow up in patients with left main coronary disease according to treatment strategies. Korean Circ J. 2003. 33:568–573.15. Baim DS, Mauri L, Cutlip DC. Drug-eluting stenting for unprotected left main coronary artery disease: are we ready to replace bypass surgery? J Am Coll Cardiol. 2006. 47:878–881.16. Barlis P, Tanigawa J, Kaplan S, di Mario C. Complex coronary interventions: unprotected left main and bifurcation lesions. J Interv Cardiol. 2006. 19:510–524.17. Black A, Cortina R, Bossi I, Choussat R, Fajadet J, Marco J. Unprotected left main coronary artery stenting: correlates of midterm survival and impact of patient selection. J Am Coll Cardiol. 2001. 37:832–838.18. Colombo A, Hall P, Nakamura S, et al. Intracoronary stenting without anticoagulation accomplished with intravascular ultrasound guidance. Circulation. 1995. 91:1676–1688.19. Schomig A, Neumann FJ, Kastrati A, et al. A ramdomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary artery stents. N Engl J Med. 1996. 334:1084–1089.20. Park SJ, Kim YH, Lee BK, et al. Sirolimus-eluting stent implantation for unprotected left main coronary artery stenosis: comparison with bare metal stent implantation. J Am Coll Cardiol. 2005. 45:351–356.21. Chieffo A, Stankovic G, Bonizzoni E, et al. Early and mid-term results of drug-eluting stent implantation in unprotected left main. Circulation. 2005. 111:791–795.22. Valgimigli M, van Mieghem CA, Ong AT, et al. Short and long-term clinical outcome after drug-eluting stent implantation for the percutaneous treatment of left main coronary artery disease: insights from the Rapamycin-Eluting and Taxus Stent Evaluated At Rotterdam Cardiology Hospital registries (RESEARCH and T-SEARCH). Circulation. 2005. 111:1383–1389.23. Lee MS, Kapoor N, Jamal F, et al. Comparison of coronary artery bypass surgery with percutaneous coronary intervention with drug-eluting stents for unprotected left main coronary artery disease. J Am Coll Cardiol. 2006. 47:864–870.24. Price MJ, Cristea E, Sawhney N, et al. Serial angiographic follow-up of sirolimus-eluting stents for unprotected left main coronary artery revascularization. J Am Coll Cardiol. 2006. 47:871–877.25. Lee CH, Degertekin M, van Domburg RT, et al. Impact of different anatomical patterns of left main coronary stenting on long-term survival. Am J Cardiol. 2003. 92:718–720.26. Wood F, Bazemore E, Schneider JE, Jobe RL, Mann T. Technique of left main stenting is dependent on lesion location and distal branch protection. Catheter Cardiovasc Interv. 2005. 65:499–503.27. Ragosta M, Dee S, Sarembock IJ, Lipson LC, Gimple LW, Powers ER. Prevalence of unfavorable angiographic characteristics for percutaneous intervention in patients with unprotected left main coronary artery disease. Catheter Cardiovasc Interv. 2006. 68:357–362.28. Ge L, Airoldi F, Iakovou I, et al. Clinical and angiographic outcome after implantation of drug-eluting stnets in bifurcation lesions with the crush stent technique: importance of final kissing balloon post-dilation. J Am Coll Cardiol. 2005. 46:613–620.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stenting of Unprotected Left Main Coronary Artery Stenosis without Anticogulation: Immediate and Late Outcomes
- Current Status and Future Perspective of Left Main Coronary Intervention
- A Case of Left Coronary Artery Milking Treated by Direct Stenting During Percutaneous Coronary Intervention in A Patient with Unstable Angina
- Early and late clinical outcomes after primary stenting of the unprotected left main coronary artery stenosis in the setting of acute myocardial infarction
- Early and Mid-term Results of Coronary Stenting in the Diabetic Patient