Korean J Hepatobiliary Pancreat Surg.
2013 Nov;17(4):152-156. 10.14701/kjhbps.2013.17.4.152.
Clinicopathological characteristics and prognostic factors in combined hepatocellular carcinoma and cholangiocarcinoma
- Affiliations
-
- 1Department of Surgery, Chonbuk National University Medical School and Hospital, Jeonju, Korea. hcyu@jbnu.ac.kr
- 2Department of Pathology, Chonbuk National University Medical School and Hospital, Jeonju, Korea.
- KMID: 2083339
- DOI: http://doi.org/10.14701/kjhbps.2013.17.4.152
Abstract
- BACKGROUNDS/AIMS
Combined hepatocellular carcinoma and cholangiocarcinoma (cHCC-CC) is an uncommon subtype of primary liver cancer that has rarely been reported in detail. This study was performed in order to evaluate the clinicopathological characteristics and prognostic factors of cHCC-CC in single center.
METHODS
The clinicopathological features of patients diagnosed and operated with cHCC-CC at Chonbuk National Hospital between July 1998 and July 2007 were retrospectively studied by comparing them with patients with only hepatocellular carcinoma (HCC) who had undergone a hepatic resection during the same period.
RESULTS
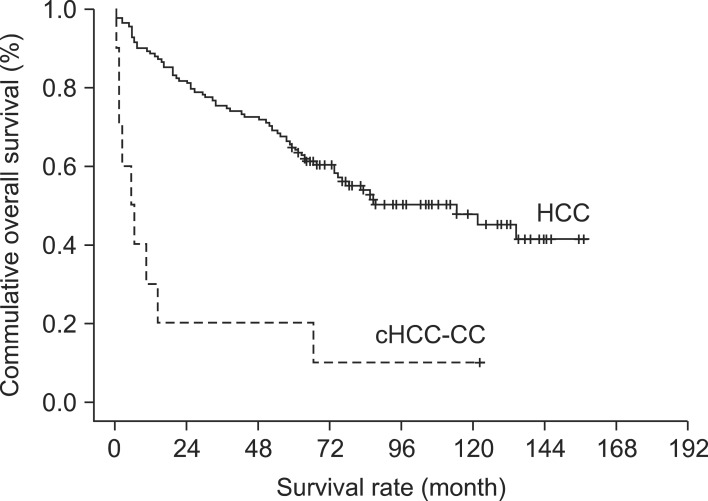
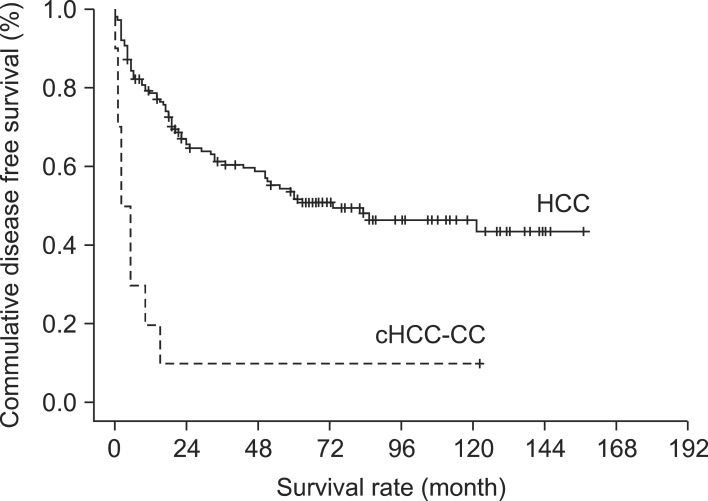
Ten out of 152 patients who had undergone a hepatic resection were diagnosed with cHCC-CC and thus included in this study (M : F=8 : 2, median age: 52+/-11.1 years). According to the parameters of the 7th American Joint Committee on Cancer T staging, there were 76 (50.0%), 44 (28.9%), 9 (5.9%), 18 (11.8%) and 5 (3.3%) patients with T stages 1, 2, 3a, 3b and 4, respectively. The overall survival period was longer in the HCC only group (68+/-40.4 months) than in the combined cHCC-CC group (23+/-40.1 months) (p<0.0001). The 5-year survival rate was 10% in the cHCC-CC group and 60% in the HCC group (p<0.0001). The disease free survival for patients with cHCC-HCC and HCC were 16+/-37.4 and 51+/-44.3 months, respectively (p<0.0001). Univariate analysis revealed that age, gender, transarterial chemoembolization (TACE), and T stage were statistically significant in terms of patient's overall survival. However, there were no significant clinicopathological factors identified by the multivariate analysis.
CONCLUSIONS
Even after the hepatic resection in the HCC, the prognosis is poorer if the patient has cholangiocellular components compared to the usual HCC.
MeSH Terms
Figure
Reference
-
1. Theise ND, Nakashima O, Park YN, Nakanuma Y. Combined hepatocellular-cholangiocarcinoma. In : Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon, France: IARC;2010. p. 225–227.2. Koh KC, Lee H, Choi MS, et al. Clinicopathologic features and prognosis of combined hepatocellular cholangiocarcinoma. Am J Surg. 2005; 189:120–125. PMID: 15701504.
Article3. Goodman ZD, Ishak KG, Langloss JM, et al. Combined hepatocellular-cholangiocarcinoma. A histologic and immunohistochemical study. Cancer. 1985; 55:124–135. PMID: 2578078.
Article4. Kim DK, Lee SM, Hong SW. Combined hepatocellular-cholangiocarcinoma. Korean J Hepatobiliary Pancreat Surg. 1998; 2:171–176.5. Yano Y, Yamamoto J, Kosuge T, et al. Combined hepatocellular and cholangiocarcinoma: a clinicopathologic study of 26 resected cases. Jpn J Clin Oncol. 2003; 33:283–287. PMID: 12913082.
Article6. Liu CL, Fan ST, Lo CM, et al. Hepatic resection for combined hepatocellular and cholangiocarcinoma. Arch Surg. 2003; 138:86–90. PMID: 12511158.
Article7. Park HS, Bae JS, Jang KY, et al. Clinicopathologic study on combined hepatocellular carcinoma and cholangiocarcinoma: with emphasis on the intermediate cell morphology. J Korean Med Sci. 2011; 26:1023–1030. PMID: 21860552.
Article8. Yin X, Zhang BH, Qiu SJ, et al. Combined hepatocellular carcinoma and cholangiocarcinoma: clinical features, treatment modalities, and prognosis. Ann Surg Oncol. 2012; 19:2869–2876. PMID: 22451237.
Article9. Maeda T, Adachi E, Kajiyama K, et al. Combined hepatocellular and cholangiocarcinoma: proposed criteria according to cytokeratin expression and analysis of clinicopathologic features. Hum Pathol. 1995; 26:956–964. PMID: 7545644.
Article10. Jarnagin WR, Weber S, Tickoo SK, et al. Combined hepatocellular and cholangiocarcinoma: demographic, clinical, and prognostic factors. Cancer. 2002; 94:2040–2046. PMID: 11932907.11. Park H, Choi KH, Choi SB, et al. Clinicopathological characteristics in combined hepatocellular-cholangiocarcinoma: a single center study in Korea. Yonsei Med J. 2011; 52:753–760. PMID: 21786439.
Article12. Okuda K. Natural history of hepatocellular carcinoma including fibrolamellar and hepato-cholangiocarcinoma variants. J Gastroenterol Hepatol. 2002; 17:401–405. PMID: 11982719.
Article13. Poon RT, Ngan H, Lo CM, et al. Transarterial chemoembolization for inoperable hepatocellular carcinoma and postresection intrahepatic recurrence. J Surg Oncol. 2000; 73:109–114. PMID: 10694648.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined Hepatocellular-Cholangiocarcinoma: Recent Progress in Pathology and Classification
- Combined Hepatocellular-cholangiocarcinoma
- Combined Hepatocellular-cholangiocarcinoma
- Clinicopathological Characteristics in Combined Hepatocellular-Cholangiocarcinoma: A Single Center Study in Korea
- Epidemiological Observation of Clonorchis sinensis Infection in Connection with Primary Carcinoma of the Liver