Korean J Obstet Gynecol.
2011 May;54(5):229-235. 10.5468/KJOG.2011.54.5.229.
Clinical usefulness of soluble fms-like tyrosine kinase 1, soluble endoglin and placental growth factor in Korean women with preeclampsia
- Affiliations
-
- 1Department of Obstetrics and Gynecology, The Catholic University of Korea College of Medicine, Seoul, Korea. ly@catholic.ac.kr
- KMID: 2078016
- DOI: http://doi.org/10.5468/KJOG.2011.54.5.229
Abstract
OBJECTIVE
To evaluate the clinical significance of soluble fms-like tyrosine kinase1 (sFlt-1), soluble endoglin (sEng) and placental growth factor (PlGF) in preeclampsia.
METHODS
We conducted a case-control study analyzing serum levels of sFlt-1, sEng and PlGF in women with preeclampsia (n=30) and normal pregnancy (n=30) in the third trimester. We calculated the sensitivity, specificity, positive, and negative predictive values of each peptide in diagnosing preeclampsia.
RESULTS
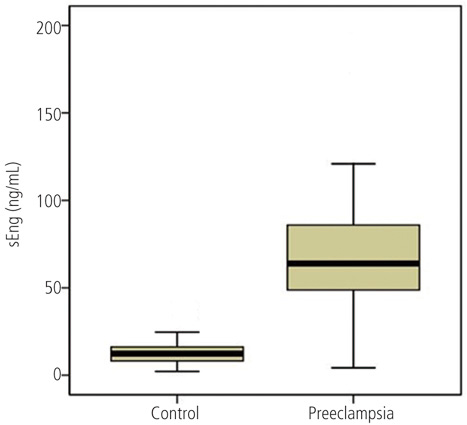
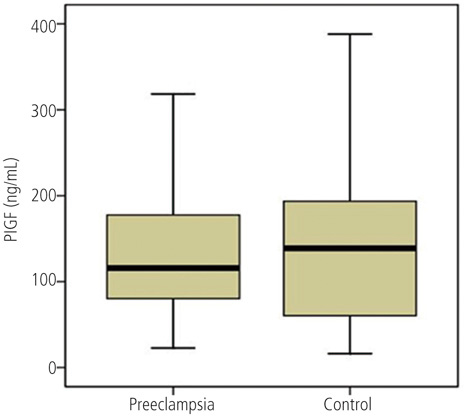
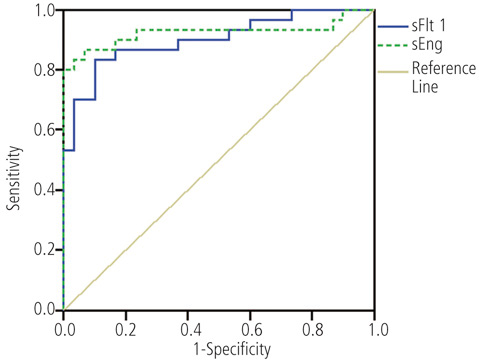
The mean serum level of sFlt-1 and sEng in women with preeclampsia was significantly higher than normal pregnancy. But the mean serum level of PIGF had no significant difference between two groups. The cut-off values of sFlt-1 and sEng showing differential significance were 26.3 ng/mL and 21.1 ng/mL each. Then the sensitivity, specificity, positive predictive value, negative predictive value was all over 80%. Serum levels of sFlt-1 and sEng were not significantly different between intrauterine growth restriction (IUGR) and non-IUGR group among preeclamptic women.
CONCLUSION
Serum levels of both sFlt-1 and sEng may be useful in diagnosing patients with preeclampsia. The serum levels of these factors may not correlate with poor perinatal outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Walker JJ. Pre-eclampsia. Lancet. 2000. 356:1260–1265.2. Redman CW, Sargent IL. Latest advances in understanding preeclampsia. Science. 2005. 308:1592–1594.3. Hauth JC, Ewell MG, Levine RJ, Esterlitz JR, Sibai B, Curet LB, et al. Calcium for Preeclampsia Prevention Study Group. Pregnancy outcomes in healthy nulliparas who developed hypertension. Obstet Gynecol. 2000. 95:24–28.4. Knuist M, Bonsel GJ, Zondervan HA, Treffers PE. Intensification of fetal and maternal surveillance in pregnant women with hypertensive disorders. Int J Gynaecol Obstet. 1998. 61:127–133.5. Sibai BM, Hauth J, Caritis S, Lindheimer MD, MacPherson C, Klebanoff M, et al. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. Hypertensive disorders in twin versus singleton gestations. Am J Obstet Gynecol. 2000. 182:938–942.6. Hnat MD, Sibai BM, Caritis S, Hauth J, Lindheimer MD, MacPherson C, et al. Perinatal outcome in women with recurrent preeclampsia compared with women who develop preeclampsia as nulliparas. Am J Obstet Gynecol. 2002. 186:422–426.7. ACOG Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol. 2002. 99:159–167.8. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000. 183:S1–S22.9. Lam C, Lim KH, Karumanchi SA. Circulating angiogenic factors in the pathogenesis and prediction of preeclampsia. Hypertension. 2005. 46:1077–1085.10. Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003. 111:649–658.11. Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004. 350:672–683.12. Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006. 12:642–649.13. Taylor RN, Grimwood J, Taylor RS, McMaster MT, Fisher SJ, North RA. Longitudinal serum concentrations of placental growth factor: evidence for abnormal placental angiogenesis in pathologic pregnancies. Am J Obstet Gynecol. 2003. 188:177–182.14. Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003. 102:181–192.15. Douglas KA, Redman CW. Eclampsia in the United Kingdom. BMJ. 1994. 309:1395–1400.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cord Blood Soluble fms-Like Tyrosine Kinase 1 and Placental Growth Factor in Preterm Infants with Maternal Preeclampsia
- Maternal Preeclampsia and Bronchopulmonary Dysplasia
- Maternal serum soluble Fas/Fas ligand level and expression of Fas/Fas ligand in placenta in preeclampsia
- Contrasting Roles of Different Endoglin Forms in Atherosclerosis
- Evaluation of sFlt-1/PlGF Ratio for Predicting and Improving Clinical Management of Pre-eclampsia: Experience in a Specialized Perinatal Care Center