Korean J Pain.
2014 Apr;27(2):125-132. 10.3344/kjp.2014.27.2.125.
Feasibility of Early and Repeated Low-dose Interscalene Brachial Plexus Block for Residual Pain in Acute Cervical Radiculopathy Treated with NSAIDS
- Affiliations
-
- 1Department of Anesthesiology, Nara Prefectural Mimuro Hospital, Nara, Japan. notkorit4ky@yahoo.co.jp
- 2Department of Anesthesiology, Heisei Memorial Hospital, Nara, Japan.
- 3Department of Anesthesiology, Nara Prefectural Nara Hospital, Nara, Japan.
- KMID: 2074058
- DOI: http://doi.org/10.3344/kjp.2014.27.2.125
Abstract
- BACKGROUND
To improve residual pain management in acute cervical radiculopathy treated with NSAIDs, the feasibility of early and repeated low-dose interscalene brachial plexus block (IS-BPB) needs to be assessed.
METHODS
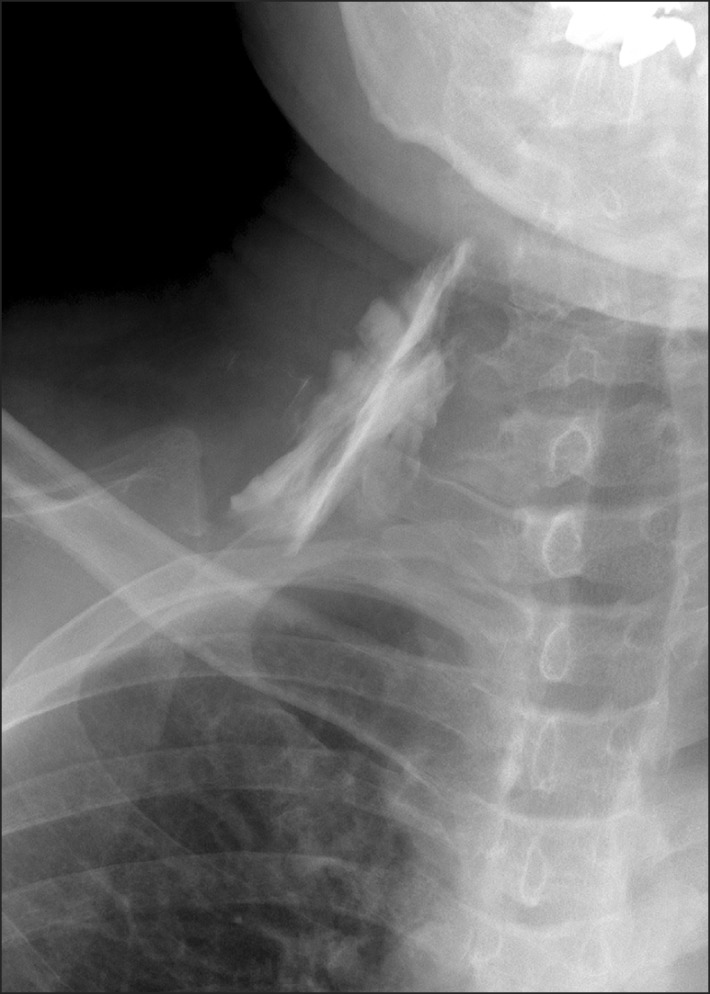
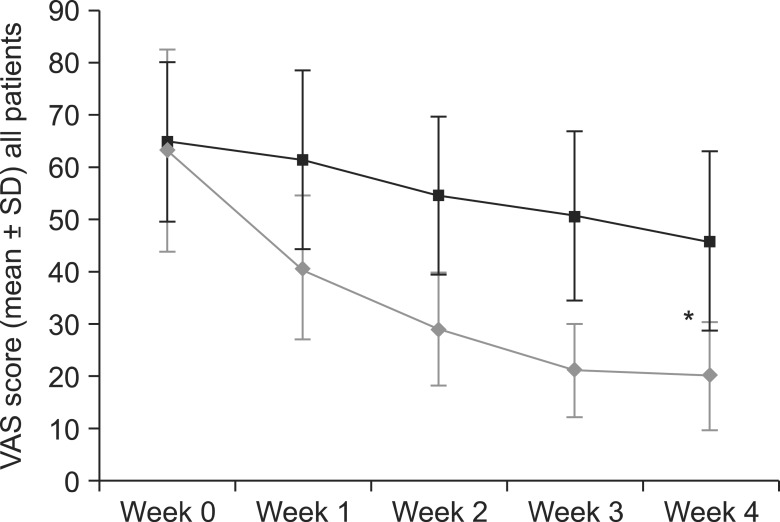
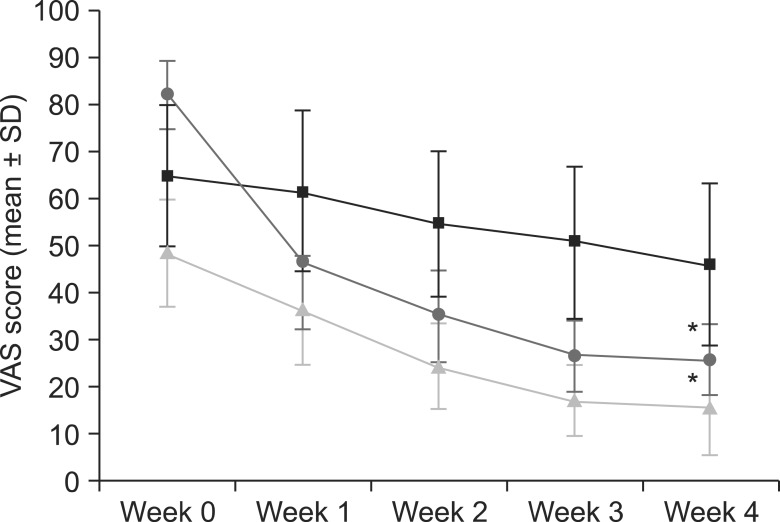
This was a prospective study on patients receiving NSAIDs (loxoprofen) for cervical radiculopathy of < or = 2-week onset. Pain was assessed using the visual analogue scale (VAS). A low-dose ultrasonography (USG)-guided IS-BPB (dexamethasone [1.65 mg; 0.5 ml] and mepivacaine [1%; 3.0 ml]) was performed at baseline and weekly thereafter for 4 weeks in an outpatient setting for the intervention group. All patients were evaluated using a visual satisfaction score (VSS) at week 4. Patients with baseline VAS scores < 70 (mild to moderate pain; MM group) and > or = 70 (severe pain; SE group) were compared to the controls receiving NSAIDs.
RESULTS
A total of 316 IS-BPBs were performed in the intervention group. There was a significant difference in the decline in the VAS from week 0 to week 3 in the MM and SE groups (P < 0.05); however, from week 3 to week 4, the therapeutic effect exhibited no significant difference. Thirteen patients at week 2 (15.5%; MM: 27.7%; SE: 0%), 43 at week 3 (51.2%; MM: 83.0%; SE: 10.8%), and 47 at week 4 (56.0%; MM: 85.1%; SE: 18.9%) achieved a VAS score of < or = 20. Patient satisfaction was high, and the decrease in VAS scores in both groups was significant (P < 0.05) compared to the controls.
CONCLUSIONS
Weekly, low-dose, USG-guided IS-BPB can be implemented for early pain relief in acute cervical radiculopathy, with high patient satisfaction.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Brachial Plexus Injury as a Complication after Nerve Block or Vessel Puncture
Hyun Jung Kim, Sang Hyun Park, Hye Young Shin, Yun Suk Choi
Korean J Pain. 2014;27(3):210-218. doi: 10.3344/kjp.2014.27.3.210.
Reference
-
1. Eubanks JD. Cervical radiculopathy: nonoperative management of neck pain and radicular symptoms. Am Fam Physician. 2010; 81:33–40. PMID: 20052961.2. Levine MJ, Albert TJ, Smith MD. Cervical radiculopathy: diagnosis and nonoperative management. J Am Acad Orthop Surg. 1996; 4:305–316. PMID: 10797198.
Article3. Dworkin RH, Backonja M, Rowbotham MC, Allen RR, Argoff CR, Bennett GJ, et al. Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol. 2003; 60:1524–1534. PMID: 14623723.4. Long TR, Wass CT, Burkle CM. Perioperative interscalene blockade: an overview of its history and current clinical use. J Clin Anesth. 2002; 14:546–556. PMID: 12477594.
Article5. Neal JM, Hebl JR, Gerancher JC, Hogan QH. Brachial plexus anesthesia: essentials of our current understanding. Reg Anesth Pain Med. 2002; 27:402–428. PMID: 12132064.
Article6. Soeding PE, Sha S, Royse CE, Marks P, Hoy G, Royse AG. A randomized trial of ultrasound-guided brachial plexus anaesthesia in upper limb surgery. Anaesth Intensive Care. 2005; 33:719–725. PMID: 16398375.
Article7. Dhir S, Ganapathy S, Lindsay P, Athwal GS. Case report: ropivacaine neurotoxicity at clinical doses in interscalene brachial plexus block. Can J Anaesth. 2007; 54:912–916. PMID: 17975237.
Article8. Krone SC, Chan VW, Regan J, Peng P, Poate EM, McCartney C, et al. Analgesic effects of low-dose ropivacaine for interscalene brachial plexus block for outpatient shoulder surgery-a dose-finding study. Reg Anesth Pain Med. 2001; 26:439–443. PMID: 11561264.
Article9. Fujimura N, Namba H, Tsunoda K, Kawamata T, Taki K, Igarasi M, et al. Effect of hemidiaphragmatic paresis caused by interscalene brachial plexus block on breathing pattern, chest wall mechanics, and arterial blood gases. Anesth Analg. 1995; 81:962–966. PMID: 7486085.
Article10. Kang SS, Jung JW, Song CK, Yoon YJ, Shin KM. A new anterior approach for fluoroscopy-guided suprascapular nerve block - a preliminary report -. Korean J Pain. 2012; 25:168–172. PMID: 22787547.
Article11. Choi IG, Choi YS, Kim YH, Min JH, Chae YK, Lee YK, et al. The effects of postoperative brachial plexus block using MgSO(4) on the postoperative pain after upper extremity surgery. Korean J Pain. 2011; 24:158–163. PMID: 21935495.
Article12. Boyce RH, Wang JC. Evaluation of neck pain, radiculopathy, and myelopathy: imaging, conservative treatment, and surgical indications. Instr Course Lect. 2003; 52:489–495. PMID: 12690875.13. Swezey RL, Swezey AM, Warner K. Efficacy of home cervical traction therapy. Am J Phys Med Rehabil. 1999; 78:30–32. PMID: 9923426.14. Persson LC, Moritz U, Brandt L, Carlsson CA. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. Eur Spine J. 1997; 6:256–266. PMID: 9294750.
Article15. Heckmann JG, Lang CJ, Zöbelein I, Laumer R, Druschky A, Neundörfer B. Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients. J Spinal Disord. 1999; 12:396–401. PMID: 10549703.16. Lees F, Turner JW. Natural history and prognosis of cervical spondylosis. Br Med J. 1963; 2:1607–1610. PMID: 14066179.
Article17. Candido KD, Knezevic N. Cervical epidural steroid injections for the treatment of cervical spinal (neck) pain. Curr Pain Headache Rep. 2013; 17:314. PMID: 23315021.
Article18. Murata Y, Kanaya K, Wada H, Wada K, Shiba M, Hatta S, et al. Interscalene brachial plexus block for scapular and upper chest pain due to cervical radiculopathy: a randomized controlled clinical trial. J Orthop Sci. 2012; 17:515–520. PMID: 22828914.
Article19. Chung JY, Yim JH, Seo HY, Kim SK, Cho KJ. The efficacy and persistence of selective nerve root block under fluoroscopic guidance for cervical radiculopathy. Asian Spine J. 2012; 6:227–232. PMID: 23275805.
Article20. Bruce BG, Green A, Blaine TA, Wesner LV. Brachial plexus blocks for upper extremity orthopaedic surgery. J Am Acad Orthop Surg. 2012; 20:38–47. PMID: 22207517.
Article21. Yuan JM, Yang XH, Fu SK, Yuan CQ, Chen K, Li JY, et al. Ultrasound guidance for brachial plexus block decreases the incidence of complete hemi-diaphragmatic paresis or vascular punctures and improves success rate of brachial plexus nerve block compared with peripheral nerve stimulator in adults. Chin Med J (Engl). 2012; 125:1811–1816. PMID: 22800905.22. Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008; 101:549–556. PMID: 18682410.
Article23. Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009; 34:498–502. PMID: 19920426.
Article24. Loubert C, Williams SR, Hélie F, Arcand G. Complication during ultrasound-guided regional block: accidental intravascular injection of local anesthetic. Anesthesiology. 2008; 108:759–760. PMID: 18362609.
Article25. Chabal C, Jacobson L, Russell LC, Burchiel KJ. Pain response to perineuromal injection of normal saline, epinephrine, and lidocaine in humans. Pain. 1992; 49:9–12. PMID: 1594285.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of Combined Superficial Cervical Plexus Block and Interscalene Brachial Plexus Block with General Anesthesia for Clavicle Surgery: Pilot Trial
- Recent updates on interscalene brachial plexus block for shoulder surgery
- Prolonged Horner's Syndrome Following Interscalene Brachial Plexus Block: A case report
- Bilateral Interscalene Brachial Plexus Block for Surgery on Both Upper Extremities in a Patient with Unilateral Vocal Cord Paralysis : A case report
- Ultrasound Guided Low Approach Interscalene Brachial Plexus Block for Upper Limb Surgery