Anesth Pain Med.
2023 Jan;18(1):5-10. 10.17085/apm.22254.
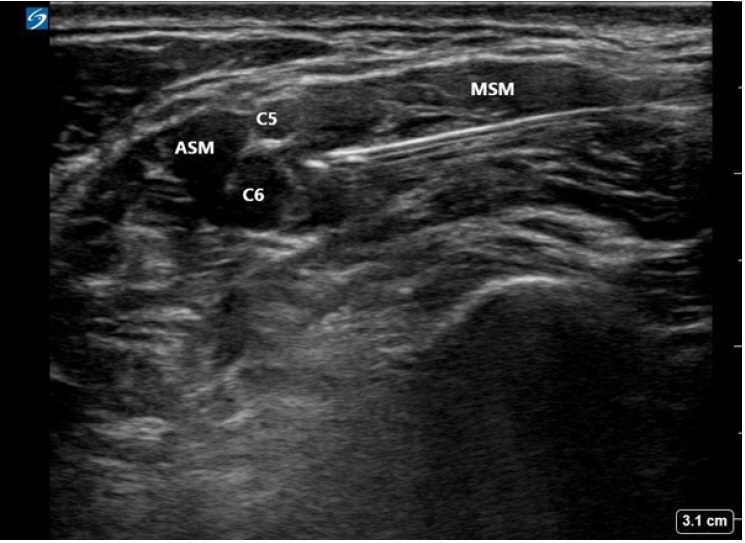
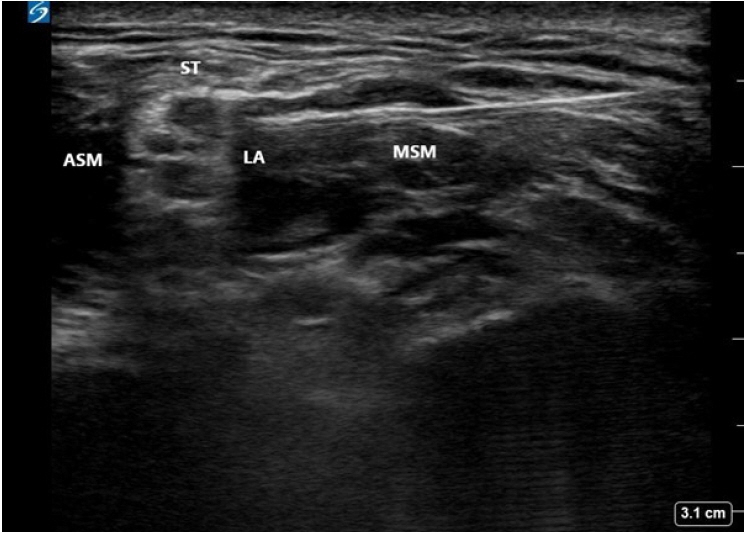
Recent updates on interscalene brachial plexus block for shoulder surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2540328
- DOI: http://doi.org/10.17085/apm.22254
Abstract
- Interscalene brachial plexus block (ISBPB) provides optimal analgesia for shoulder surgery. However, several limitations still exist, including the short duration of analgesia, rebound pain, a high incidence of unilateral diaphragmatic paresis, and potential risk of nerve damage, prompting the search for alternative techniques. Many alternatives to ISBPB have been studied to alleviate these concerns, and clinicians should choose an appropriate option based on the patient’s condition. In this mini-review, we aimed to present recent updates on ISBPB while discussing our clinical experiences in shoulder surgery.
Keyword
Figure
Reference
-
1. Mojica JJ, Ocker A, Barrata J, Schwenk ES. Anesthesia for the patient undergoing shoulder surgery. Clin Sports Med. 2022; 41:219–31.
Article2. Abdallah FW, Halpern SH, Aoyama K, Brull R. Will the real benefits of single-shot interscalene block please stand Up? A systematic review and meta-analysis. Anesth Analg. 2015; 120:1114–29.
Article3. Barry GS, Bailey JG, Sardinha J, Brousseau P, Uppal V. Factors associated with rebound pain after peripheral nerve block for ambulatory surgery. Br J Anaesth. 2021; 126:862–71.
Article4. El-Boghdadly K, Chin KJ, Chan VWS. Phrenic nerve palsy and regional anesthesia for shoulder surgery: anatomical, physiologic, and clinical considerations. Anesthesiology. 2017; 127:173–91.5. Rajpal G, Winger DG, Cortazzo M, Kentor ML, Orebaugh SL. Neurologic outcomes after low-volume, ultrasound-guided interscalene block and ambulatory shoulder surgery. Reg Anesth Pain Med. 2016; 41:477–81.
Article6. Kang R, Jeong JS, Chin KJ, Yoo JC, Lee JH, Choi SJ, et al. Superior trunk block provides noninferior analgesia compared with interscalene brachial plexus block in arthroscopic shoulder surgery. Anesthesiology. 2019; 131:1316–26.
Article7. Kang R, Jeong JS, Yoo JC, Lee JH, Choi SJ, Gwak MS, et al. Effective dose of intravenous dexmedetomidine to prolong the analgesic duration of interscalene brachial plexus block: a single-center, prospective, double-blind, randomized controlled trial. Reg Anesth Pain Med. 2018; 43:488–95.8. Kang RA, Jeong JS, Yoo JC, Lee JH, Gwak MS, Choi SJ, et al. Improvement in postoperative pain control by combined use of intravenous dexamethasone with intravenous dexmedetomidine after interscalene brachial plexus block for arthroscopic shoulder surgery: a randomised controlled trial. Eur J Anaesthesiol. 2019; 36:360–8.9. Vorobeichik L, Brull R, Bowry R, Laffey JG, Abdallah FW. Should continuous rather than single-injection interscalene block be routinely offered for major shoulder surgery? A meta-analysis of the analgesic and side-effects profiles. Br J Anaesth. 2018; 120:679–92.
Article10. Abdallah FW, Dwyer T, Chan VW, Niazi AU, Ogilvie-Harris DJ, Oldfield S, et al. IV and perineural dexmedetomidine similarly prolong the duration of analgesia after interscalene brachial plexus block: a randomized, three-arm, triple-masked, placebo-controlled trial. Anesthesiology. 2016; 124:683–95.11. Patel MA, Gadsden JC, Nedeljkovic SS, Bao X, Zeballos JL, Yu V, et al. Brachial plexus block with liposomal bupivacaine for shoulder surgery improves analgesia and reduces opioid consumption: results from a multicenter, randomized, double-blind, controlled trial. Pain Med. 2020; 21:387–400.
Article12. Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011; 113:904–25.13. Fredrickson MJ, Leightley P, Wong A, Chaddock M, Abeysekera A, Frampton C. An analysis of 1505 consecutive patients receiving continuous interscalene analgesia at home: a multicentre prospective safety study. Anaesthesia. 2016; 71:373–9.
Article14. Williams BA, Hough KA, Tsui BY, Ibinson JW, Gold MS, Gebhart GF. Neurotoxicity of adjuvants used in perineural anesthesia and analgesia in comparison with ropivacaine. Reg Anesth Pain Med. 2011; 36:225–30.
Article15. Woo JH, Kim YJ, Kim DY, Cho S. Dose-dependency of dexamethasone on the analgesic effect of interscalene block for arthroscopic shoulder surgery using ropivacaine 0.5%: a randomised controlled trial. Eur J Anaesthesiol. 2015; 32:650–5.16. Jung HS, Seo KH, Kang JH, Jeong JY, Kim YS, Han NR. Optimal dose of perineural dexmedetomidine for interscalene brachial plexus block to control postoperative pain in patients undergoing arthroscopic shoulder surgery: a prospective, double-blind, randomized controlled study. Medicine (Baltimore). 2018; 97:e0440.17. Hussain N, Brull R, Sheehy B, Essandoh MK, Stahl DL, Weaver TE, et al. Perineural liposomal bupivacaine is not superior to nonliposomal bupivacaine for peripheral nerve block analgesia. Anesthesiology. 2021; 134:147–64.
Article18. Prabhakar A, Ward CT, Watson M, Sanford J, Fiza B, Moll V, et al. Liposomal bupivacaine and novel local anesthetic formulations. Best Pract Res Clin Anaesthesiol. 2019; 33:425–32. Erratum in: Best Pract Res Clin Anaesthesiol 2021; 35: E1-2.
Article19. Ilfeld BM. Liposome bupivacaine in peripheral nerve blocks and epidural injections to manage postoperative pain. Expert Opin Pharmacother. 2013; 14:2421–31.
Article20. Vandepitte C, Kuroda M, Witvrouw R, Anne L, Bellemans J, Corten K, et al. Addition of liposome bupivacaine to bupivacaine HCl versus bupivacaine HCl alone for interscalene brachial plexus block in patients having major shoulder surgery. Reg Anesth Pain Med. 2017; 42:334–41.
Article21. Kim DH, Liu J, Beathe JC, Lin Y, Wetmore DS, Kim SJ, et al. Interscalene brachial plexus block with liposomal bupivacaine versus standard bupivacaine with perineural dexamethasone: a noninferiority trial. Anesthesiology. 2022; 136:434–47. Erratum in: Anesthesiology 2022. doi: 10.1097/ALN.0000000000004255.22. Muñoz-Leyva F, Cubillos J, Chin KJ. Managing rebound pain after regional anesthesia. Korean J Anesthesiol. 2020; 73:372–83.
Article23. Woo JH, Lee HJ, Oh HW, Lee JW, Baik HJ, Kim YJ. Perineural dexamethasone reduces rebound pain after ropivacaine single injection interscalene block for arthroscopic shoulder surgery: a randomized controlled trial. Reg Anesth Pain Med. 2021; 46:965–70.
Article24. Kim DH, Lin Y, Beathe JC, Liu J, Oxendine JA, Haskins SC, et al. Superior trunk block: a phrenic-sparing alternative to the interscalene block: a randomized controlled trial. Anesthesiology. 2019; 131:521–33.25. Albrecht E, Bathory I, Fournier N, Jacot-Guillarmod A, Farron A, Brull R. Reduced hemidiaphragmatic paresis with extrafascial compared with conventional intrafascial tip placement for continuous interscalene brachial plexus block: a randomized, controlled, double-blind trial. Br J Anaesth. 2017; 118:586–92.
Article26. Hussain N, Costache I, Kumar N, Essandoh M, Weaver T, Wong P, et al. Is supraclavicular block as good as interscalene block for acute pain control following shoulder surgery? A systematic review and meta-analysis. Anesth Analg. 2020; 130:1304–19.
Article27. Kang RA, Chung YH, Ko JS, Yang MK, Choi DH. Reduced hemidiaphragmatic paresis with a "corner pocket" technique for supraclavicular brachial plexus block: single-center, observer-blinded, randomized controlled trial. Reg Anesth Pain Med. 2018; 43:720–4.28. Burckett-St Laurent D, Chan V, Chin KJ. Refining the ultrasound-guided interscalene brachial plexus block: the superior trunk approach. Can J Anaesth. 2014; 61:1098–102.
Article29. Tran J, Peng PWH, Agur AMR. Anatomical study of the innervation of glenohumeral and acromioclavicular joint capsules: implications for image-guided intervention. Reg Anesth Pain Med. 2019; doi: 10.1136/rapm-2018-100152. [Epub ahead of print].
Article30. Price DJ. The shoulder block: a new alternative to interscalene brachial plexus blockade for the control of postoperative shoulder pain. Anaesth Intensive Care. 2007; 35:575–81.
Article31. Laumonerie P, Dalmas Y, Tibbo ME, Robert S, Faruch M, Chaynes P, et al. Sensory innervation of the human shoulder joint: the three bridges to break. J Shoulder Elbow Surg. 2020; 29:e499–507.
Article32. Rhyner P, Kirkham K, Hirotsu C, Farron A, Albrecht E. A randomised controlled trial of shoulder block vs. interscalene brachial plexus block for ventilatory function after shoulder arthroscopy. Anaesthesia. 2020; 75:493–8.
Article33. Sun C, Zhang X, Ji X, Yu P, Cai X, Yang H. Suprascapular nerve block and axillary nerve block versus interscalene nerve block for arthroscopic shoulder surgery: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2021; 100:e27661.34. Abdallah FW, Wijeysundera DN, Laupacis A, Brull R, Mocon A, Hussain N, et al. Subomohyoid anterior suprascapular block versus interscalene block for arthroscopic shoulder surgery: a multicenter randomized trial. Anesthesiology 2020; 132: 839-53. Erratum in: Anesthesiology. 2020; 132:1619.35. Hussain N, Goldar G, Ragina N, Banfield L, Laffey JG, Abdallah FW. Suprascapular and interscalene nerve block for shoulder surgery: a systematic review and meta-analysis. Anesthesiology. 2017; 127:998–1013.36. Berg AA, Flaherty JM, Habeck JM, Harrison AK, Braman JP, Kaizer AM, et al. Evaluation of diaphragmatic function after interscalene block with liposomal bupivacaine: a randomized controlled trial. Anesthesiology. 2022; 136:531–41.
Article37. Franco CD, Williams JM. Ultrasound-guided interscalene block: reevaluation of the "stoplight" sign and clinical implications. Reg Anesth Pain Med. 2016; 41:452–9.38. Orebaugh SL, McFadden K, Skorupan H, Bigeleisen PE. Subepineurial injection in ultrasound-guided interscalene needle tip placement. Reg Anesth Pain Med. 2010; 35:450–4.
Article39. Kim YD, Yu JY, Shim J, Heo HJ, Kim H. Risk of encountering dorsal scapular and long thoracic nerves during ultrasound-guided interscalene brachial plexus block with nerve stimulator. Korean J Pain. 2016; 29:179–84.
Article40. Harbell MW, Kolodzie K, Behrends M, Ma CB, Kinjo S, Yap E, et al. Extraplexus versus intraplexus ultrasound-guided interscalene brachial plexus block for ambulatory arthroscopic shoulder surgery: a randomized controlled trial. PLoS One. 2021; 16:e0246792.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prolonged Horner's Syndrome Following Interscalene Brachial Plexus Block: A case report
- Pleural effusion and atelectasis during continuous interscalene brachial plexus block: A case report
- A clinical comparison of continuous interscalene brachial plexus block with different basal infusion rates of 0.2% ropivacaine for shoulder surgery
- Interscalene Brachial Plexus Block Following Suprascapular Nerve Block for Humeral Head Surgery in a Patient with Difficult Supine Position: A case report
- Ultrasound Guided Low Approach Interscalene Brachial Plexus Block for Upper Limb Surgery