Korean J Perinatol.
2015 Mar;26(1):12-20. 10.14734/kjp.2015.26.1.12.
Delivery Room Management: First Step to the Best Neonatal Outcome
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Boramae Hospital, Seoul, Korea. ljinna@snu.ac.kr
- KMID: 2072332
- DOI: http://doi.org/10.14734/kjp.2015.26.1.12
Abstract
- Delivery room management is the first step to the intact survival of preterm infants, especially in the first hour of an infant's life following delivery, "a golden hour". Admission temperature within a range of 36.5degrees C to 37.4degrees C, delayed umbilical cord clamping and cord milking, minimal oxygen supplementation, and prophylactic continuous positive airway pressure or surfactant without intubation are the cornerstones of recent delivery room management. Such managements can be supplied only by team approach including obstetrician, neonatologist, and nurses.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Risk Factors Associated with Hypothermia Immediately after Birth among Preterm Infants
Jaewoo An, Bo Kyeong Jin, Heui Seung Jo, Hye-Rim Kim, Kee Hyun Cho, Kyu Hyung Lee
Perinatology. 2018;29(1):20-26. doi: 10.14734/PN.2018.29.01.20.
Reference
-
References
1. Wyckoff MH. Initial resuscitation and stabilization of the periviable neonate: the Golden-Hour approach. Semin Perinatol. 2014; 38:12–6.
Article2. Wyckoff MH, Salhab WA, Heyne RJ, Kendrick DE, Stoll BJ, Laptook AR. Outcome of extremely low birth weight infants who received delivery room cardiopulmonary resuscitation. J Pediatr. 2012; 160:239–44.
Article3. Laptook AR, Salhab W, Bhaskar B. Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatrics. 2007; 119:e643–9.
Article4. Castrodale V, Rinehart S. The golden hour: improving the stabilization of the very low birthweight infant. Adv Neonatal Care. 2014; 14:9–14.5. Bissinger RL, Annibale DJ. Thermoregulation in very low-birthweight infants during the golden hour: results and implications. Adv Neonatal Care. 2010; 10:230–8.7. Yao AC, Moinian M, Lind J. Distribution of blood between infant and placenta after birth. Lancet. 1969; 2:871–3.
Article8. Hosono S, Hine K, Nagano N, Taguchi Y, Yoshikawa K, Okada T, et al. Residual blood volume in the umbilical cord of extremely premature infants. Pediatr Int. 2015; 57:68–71.
Article9. Vain NE, Satragno DS, Gorenstein AN, Gordillo JE, Berazategui JP, Alda MG, et al. Effect of gravity on volume of placental transfusion: a multicentre, randomised, non-inferiority trial. Lancet. 2014; 384:235–40.
Article10. Rabe H, Diaz-Rossello JL, Duley L, Dowswell T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2012; 8:CD003248.
Article11. Ghavam S, Batra D, Mercer J, Kugelman A, Hosono S, Oh W, et al. Effects of placental transfusion in extremely low birthweight infants: metaanalysis of long- and short-term outcomes. Transfusion. 2014; 54:1192–8.
Article12. Backes CH, Rivera BK, Haque U, Bridge JA, Smith CV, Hutchon DJ, et al. Placental transfusion strategies in very preterm neonates: a systematic review and metaanalysis. Obstet Gynecol. 2014; 124:47–56.13. Raju TN. Timing of umbilical cord clamping after birth for optimizing placental transfusion. Curr Opin Pediatr. 2013; 25:180–7.
Article14. Rabi Y, Dawson JA. Oxygen therapy and oximetry in the delivery room. Semin Fetal Neonatal Med. 2013; 18:330–5.
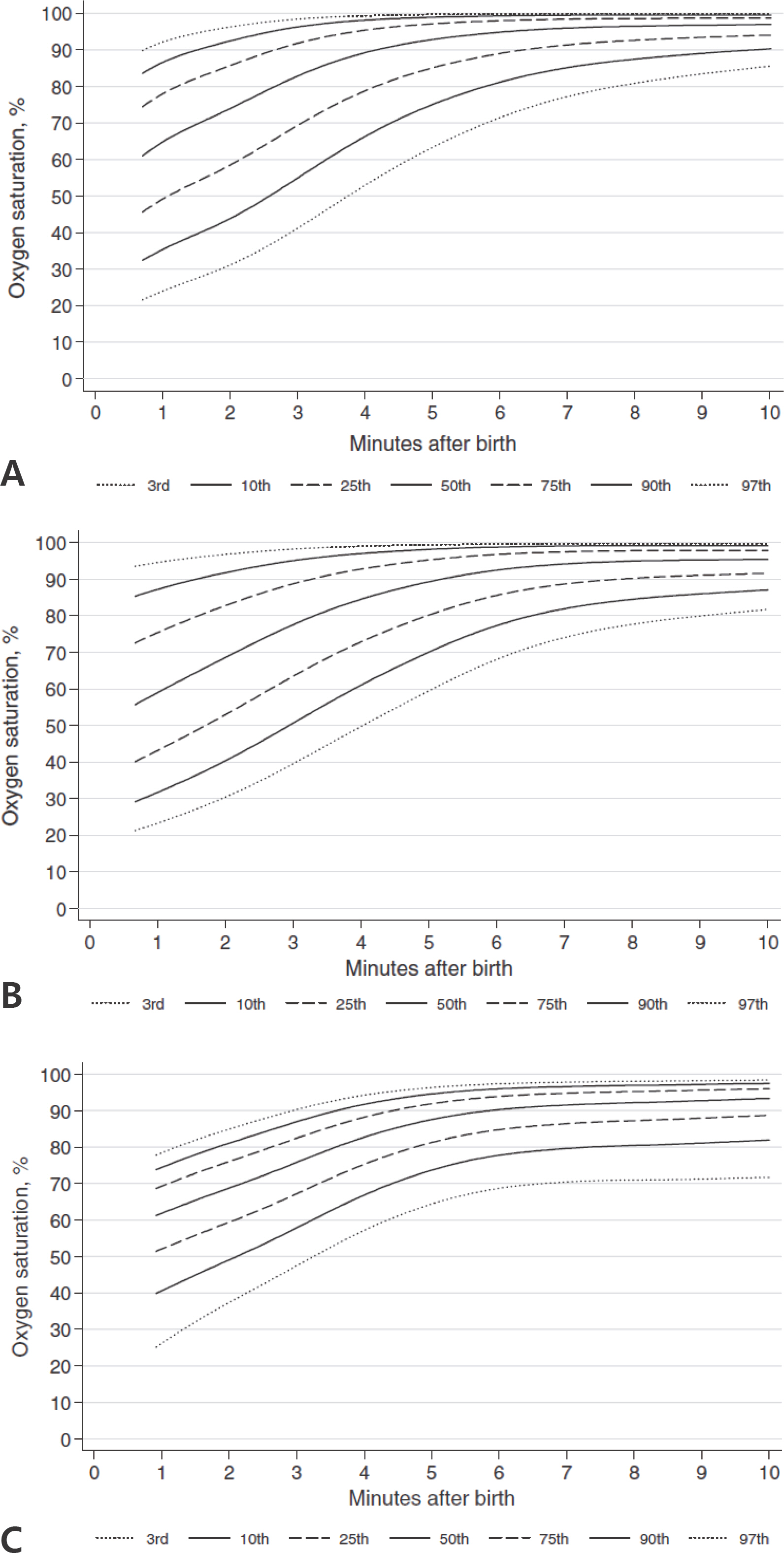
Article15. Dawson JA, Kamlin CO, Vento M, Wong C, Cole TJ, Donath SM, et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics. 2010; 125:e1340–7.
Article16. Gandhi B, Rich W, Finer N. Achieving targeted pulse oximetry values in preterm infants in the delivery room. J Pediatr. 2013; 163:412–5.
Article17. Vento M, Moro M, Escrig R, Arruza L, Villar G, Izquierdo I, et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics. 2009; 124:e439–49.
Article18. Saugstad OD, Ramji S, Soll RF, Vento M. Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and metaanalysis. Neonatology. 2008; 94:176–82.19. Saugstad OD, Aune D, Aguar M, Kapadia V, Finer N, Vento M. Systematic review and metaanalysis of optimal initial fraction of oxygen levels in the delivery room at </=32 weeks. Acta paediatr. 2014; 103:744–51.20. Kapadia VS, Chalak LF, Sparks JE, Allen JR, Savani RC, Wyckoff MH. Resuscitation of preterm neonates with limited versus high oxygen strategy. Pediatrics. 2013; 132:e1488–96.
Article21. Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European consensus guidelines on the management of neonatal respiratory distress syndrome in preterm infants–2013 update. Neonatology. 2013; 103:353–68.22. Vento M, Cubells E, Escobar JJ, Escrig R, Aguar M, Brugada M, et al. Oxygen saturation after birth in preterm infants treated with continuous positive airway pressure and air: assessment of gender differences and comparison with a published nomogram. Arch Dis Child Fetal Neonatal Ed. 2013; 98:F228–32.
Article23. Rojas-Reyes MX, Morley CJ, Soll R. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2012; 3:CD000510.
Article24. Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010; 362:1970–9.
Article25. Vaucher YE, Peralta-Carcelen M, Finer NN, Carlo WA, Gantz MG, Walsh MC, et al. Neurodevelopmental outcomes in the early CPAP and pulse oximetry trial. N Engl J Med. 2012; 367:2495–504.
Article26. Polin RA, Carlo WA. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics. 2014; 133:156–63.
Article27. Respiratory support in preterm infants at birth. Pediatrics. 2014; 133:171–4.28. Dargaville PA, Aiyappan A, De Paoli AG, Kuschel CA, Kamlin CO, Carlin JB, et al. Minimally-invasive surfactant therapy in preterm infants on continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 2013; 98:F122–6.
Article29. Kanmaz HG, Erdeve O, Canpolat FE, Mutlu B, Dilmen U. Surfactant administration via thin catheter during spontaneous breathing: randomized controlled trial. Pediatrics. 2013; 131:e502–9.
Article30. Lista G, Fontana P, Castoldi F, Cavigioli F, Dani C. Does sustained lung inflation at birth improve outcome of preterm infants at risk for respiratory distress syndrome? Neonatology. 2011; 99:45–50.
Article31. te Pas AB, Walther FJ. A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics. 2007; 120:322–9.
Article32. Dani C, Lista G, Pratesi S, Boni L, Agosti M, Biban P, et al. Sustained lung inflation in the delivery room in preterm infants at high risk of respiratory distress syndrome (SLI STUDY): study protocol for a randomized controlled trial. Trials. 2013; 14:67.
Article33. Kapadia VS, Wyckoff MH. Drugs during delivery room resuscitation–what, when and why? Semin Fetal Neonatal Med. 2013; 18:357–61.34. Lista G, Fontana P, Castoldi F, Cavigioli F, Bianchi S, Bastrenta P. ELBW infants: to intubate or not to intubate in the delivery room? J Matern Fetal Neonatal Med. 2012; 25(Suppl 4):63–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Work Experiences of Delivery Room Nurses: A Phenomenological Study
- A Study on Stress of the Nursing Student in Delivery Room Practice
- Neonatal outcome of vertex-vertex and vertex-nonvertex second twin according to the mode of delivery
- Comparison of Pregnancy Prognosis for Gestational Diabetes Diagnosed by the 1-Step and 2-Step Methods
- The perinatal outcome of vaginal delivery in twin pregnancy