Yonsei Med J.
2014 Nov;55(6):1743-1746. 10.3349/ymj.2014.55.6.1743.
Usefulness of Permanent Tracheostoma in Chronic Brain Injured Patients: A Case Series
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Chonbuk National University Medical School, Jeonju, Korea.
- 2Department of Rehabilitation, Hanyang University Medical Center, Seoul, Korea.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, School of Medicine, Ewha Womans University, Seoul, Korea.
- 4Department of Rehabilitation Medicine, School of Medicine, Ewha Womans University, Seoul, Korea. acebhs@gmail.com
- KMID: 2070226
- DOI: http://doi.org/10.3349/ymj.2014.55.6.1743
Abstract
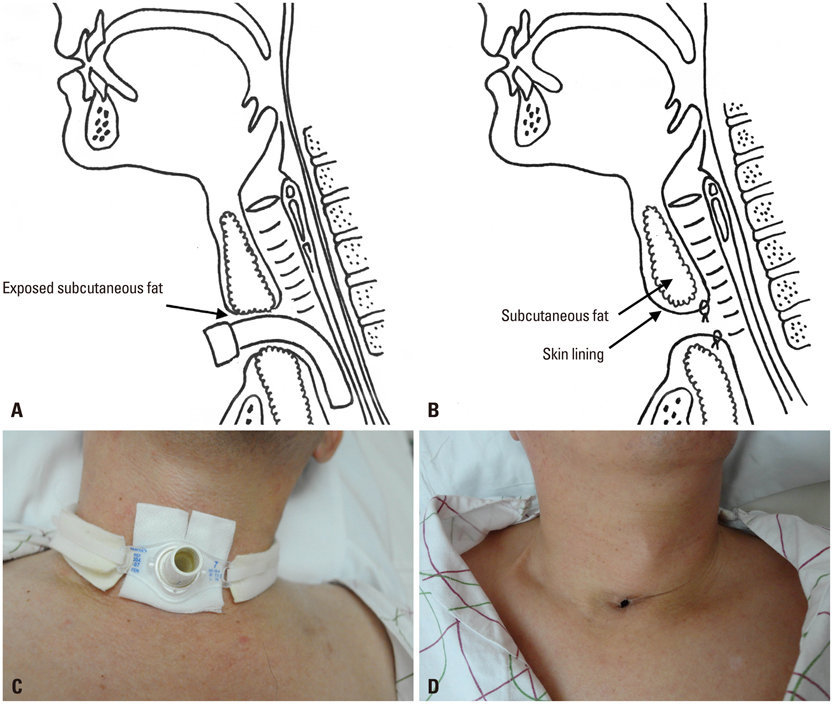
- Patients with severe neurological deficit, such as hypoxic ischemic injury, cerebral infarction, and traumatic brain injury, often show comatose mental status and require maintenance of long-term tracheostomy for pulmonary toileting. However, several complications, which are mostly related to the cannula, invariably occur. Permanent tracheostoma is a short, skin-lined, noncollapsing, self-sustaining opening by suturing the denuded skin lining to the margin of the tracheal stoma. This tube-free method is a useful alternative to make long-term airway without tube-related complications in chronic diseases, such as obstructive sleep apnea, and laryngeal cancer, however, it has not yet been reported in chronic brain injured patients. This case report illustrates 3 cases of vegetative patients in our rehabilitation clinic who underwent successful procedure of permanent tracheostoma. Permanent tracheostoma has some benefits associated with the free of tube-related complications, and can be considered as a useful alternative way for chronic brain injured patients with long-term tracheostomy.
MeSH Terms
Figure
Reference
-
1. Lee DJ, Chun MH. The effects of tracheostomy for the functional outcomes of severe traumatic brain injury patients. J Korean Acad Rehabil Med. 1998; 22:811–815.2. Woo P, Kelly G, Kirshner P. Airway complications in the head injured. Laryngoscope. 1989; 99(7 Pt 1):725–731.
Article3. Chew JY, Cantrell RW. Tracheostomy. Complications and their management. Arch Otolaryngol. 1972; 96:538–545.
Article4. Law JH, Barnhart K, Rowlett W, de la Rocha O, Lowenberg S. Increased frequency of obstructive airway abnormalities with long-term tracheostomy. Chest. 1993; 104:136–138.
Article5. Wetmore RF, Handler SD, Potsic WP. Pediatric tracheostomy. Experience during the past decade. Ann Otol Rhinol Laryngol. 1982; 91(6 Pt 1):628–632.6. Crysdale WS, Feldman RI, Naito K. Tracheotomies: a 10-year experience in 319 children. Ann Otol Rhinol Laryngol. 1988; 97(5 Pt 1):439–443.
Article7. Eliachar I, Zohar S, Golz A, Joachims HZ, Goldsher M. Permanent tracheostomy. Head Neck Surg. 1984; 7:99–103.
Article8. Eliachar I, Stegmoyer RJ, Levine HL, Sivak ED, Mehta AC, Tucker HM. Planning and management of long-standing tracheostomy. Otolaryngol Head Neck Surg. 1987; 97:385–390.
Article9. Eliachar I. Unaided speech in long-term tube-free tracheostomy. Laryngoscope. 2000; 110(5 Pt 1):749–760.
Article10. Eliachar I, Akst LM, Eliashar R. Unaided speech in tube-free tracheostomy: The supplementary sling procedure. Otolaryngol Head Neck Surg. 2002; 127:213–220.
Article11. Fee WE Jr, Ward PH. Permanent tracheostomy: a new surgical technique. Ann Otol Rhinol Laryngol. 1977; 86(5 Pt 1):635–638.12. Eliashar R, Goldfarb A, Gross M, Sichel JY. A permanent tube-free tracheostomy in a morbidly obese patient with severe obstructive sleep apnea syndrome. Isr Med Assoc J. 2002; 4:1156–1157.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of Total Laryngectomy on spinal Cord Dosein Advanced Laryngeal Cancers
- Pectoralis Major Musculocutaneous Flap for Reconstruction of Permanent Tracheostoma
- Lysophosphatidic Acid Receptor 1 Plays a Pathogenic Role in Permanent Brain Ischemic Stroke by Modulating Neuroinflammatory Responses
- Closure of VSD in a Patient with Tracheostoma: A case report
- Changes of Respiratory Patterns Associated with Swallowing in Brain-injured Patients