J Korean Med Sci.
2014 Nov;29(11):1577-1582. 10.3346/jkms.2014.29.11.1577.
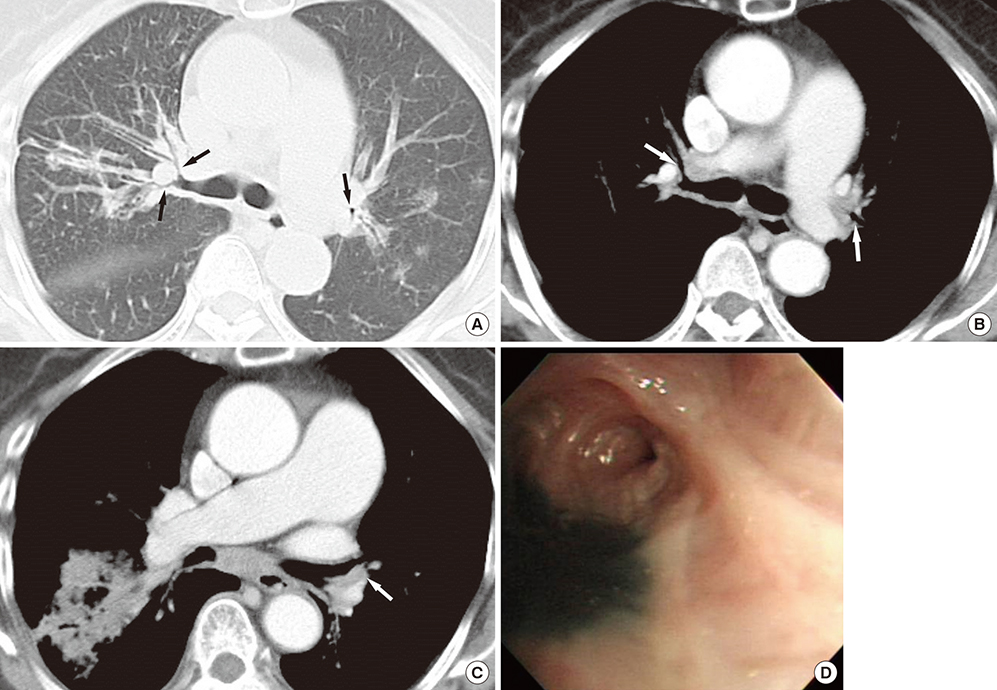
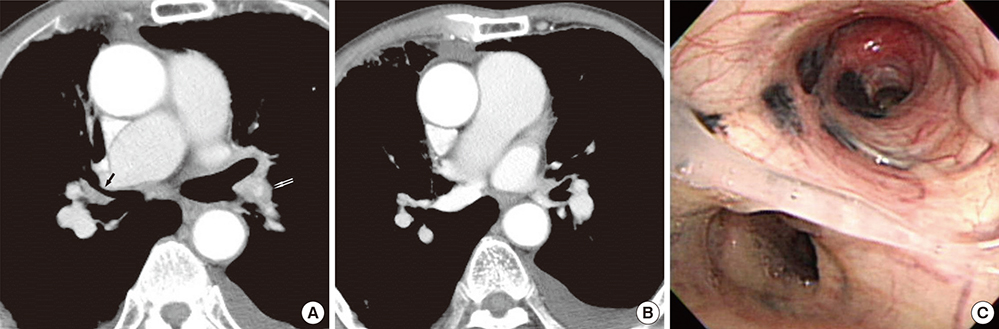
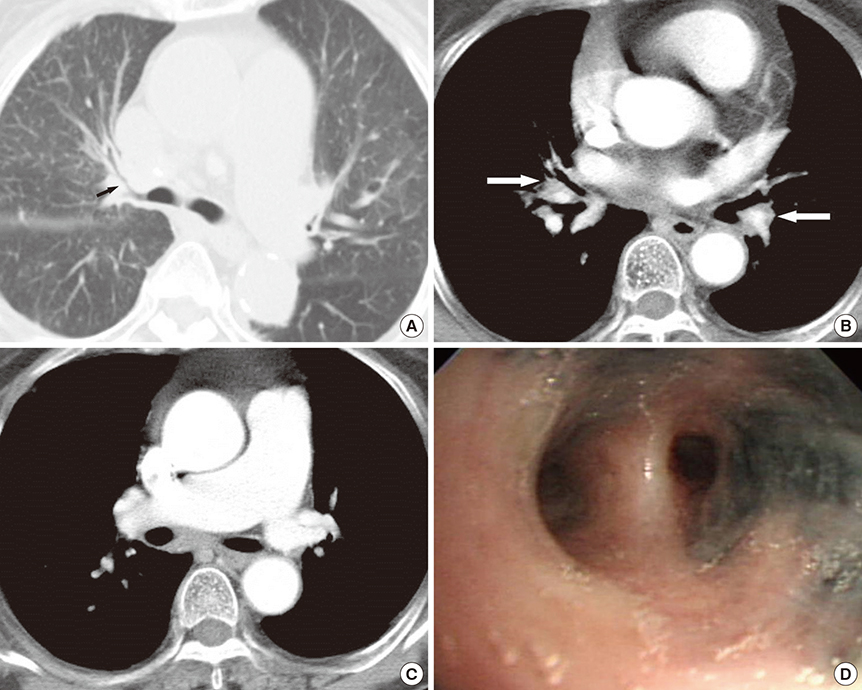
Main Pulmonary Artery Dilatation in Patients with Anthracofibrosis
- Affiliations
-
- 1Department of Radiology, Collage of Medicine, The Catholic University of Korea, St. Vincent's Hospital, Suwon, Korea. radiodoc@catholic.ac.kr
- KMID: 2069942
- DOI: http://doi.org/10.3346/jkms.2014.29.11.1577
Abstract
- This study assessed main pulmonary artery diameter of patients with anthracofibrosis. Patients with anthracofibrosis and CT scans were evaluated after exclusion of patients with co-existing disease. We measured the diameter of the main pulmonary artery (PAD) and ascending aorta (AD) and calculated the pulmonary artery to aorta ratio (APR). The upper reference limit for comparison of PAD was 29 mm. Cut-off values for PAD and APR indicating pulmonary hypertension were 33 mm and 1. We correlated the CT parameters with echocardiographic results. Total 51 patients were included in the analysis. The mean PAD, AD, and APR were 33 mm, 38 mm, and 0.87 respectively. The PAD was larger than the upper reference limit, 29 mm (P<0.001). The PAD was >33 mm in 30 (65%) and the APR was >1 in 9 patients (18%). Of 21 patients with echocardiography, 11 (52%) were found to have pulmonary hypertension. There was no statistical difference in the diagnosis of pulmonary hypertension between echocardiography and CT (P=1.000). In conclusion, main pulmonary artery is dilated in patients with anthracofibrosis more than in the healthy population.
MeSH Terms
Figure
Reference
-
1. Tan RT, Kuzo R, Goodman LR, Siegel R, Haasler GB, Presberg KW. Utility of CT scan evaluation for predicting pulmonary hypertension in patients with parenchymal lung disease. Medical College of Wisconsin Lung Transplant Group. Chest. 1998; 113:1250–1256.2. Edwards PD, Bull RK, Coulden R. CT measurement of main pulmonary artery diameter. Br J Radiol. 1998; 71:1018–1020.3. Rubin LJ. Primary pulmonary hypertension. Chest. 1993; 104:236–250.4. Rich S. Clinical insights into the pathogenesis of primary pulmonary hypertension. Chest. 1998; 114:237s–241s.5. McGoon M, Gutterman D, Steen V, Barst R, McCrory DC, Fortin TA, Loyd JE. American College of Chest Physicians. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004; 126:14s–34s.6. Devaraj A, Wells AU, Meister MG, Corte TJ, Wort SJ, Hansell DM. Detection of pulmonary hypertension with multidetector CT and echocardiography alone and in combination. Radiology. 2010; 254:609–616.7. Sandoval J, Salas J, Martinez-Guerra ML, Gómez A, Martinez C, Portales A, Palomar A, Villegas M, Barrios R. Pulmonary arterial hypertension and cor pulmonale associated with chronic domestic woodsmoke inhalation. Chest. 1993; 103:12–20.8. Moran-Mendoza O, Pérez-Padilla JR, Salazar-Flores M, Vazquez-Alfaro F. Wood smoke-associated lung disease: a clinical, functional, radiological and pathological description. Int J Tuberc Lung Dis. 2008; 12:1092–1098.9. Chung MP, Lee KS, Han J, Kim H, Rhee CH, Han YC, Kwon OJ. Bronchial stenosis due to anthracofibrosis. Chest. 1998; 113:344–350.10. Kim HY, Im JG, Goo JM, Kim JY, Han SK, Lee JK, Song JW. Bronchial anthracofibrosis (inflammatory bronchial stenosis with anthracotic pigmentation): CT findings. AJR Am J Roentgenol. 2000; 174:523–527.11. Kim YJ, Jung CY, Shin HW, Lee BK. Biomass smoke induced bronchial anthracofibrosis: presenting features and clinical course. Respir Med. 2009; 103:757–765.12. Naccache JM, Monnet I, Nunes H, Billon-Galland MA, Pairon JC, Guillon F, Valeyre D. Anthracofibrosis attributed to mixed mineral dust exposure: report of three cases. Thorax. 2008; 63:655–657.13. Kim MH, Lee HY, Nam KH, Lim JM, Jung BH, Ryu DS. The clinical significance of bronchial anthracofibrosis associated with coal workers' pneumoconiosis. Tuberc Respir Dis. 2010; 68:67–73.14. Karazincir S, Balci A, Seyfeli E, Akoğlu S, Babayiğit C, Akgül F, Yalcin F, Eğilmez E. CT assessment of main pulmonary artery diameter. Diagn Interv Radiol. 2008; 14:72–74.15. Guthaner DF, Wexler L, Harell G. CT demonstration of cardiac structures. AJR Am J Roentgenol. 1979; 133:75–81.16. Gotway MB. Pulmonary hypertension. In : Webb WR, Higgins CB, editors. Thoracic imaging: pulmonary and cardiovascular radiology. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins;2011. p. 683–699.17. Kuriyama K, Gamsu G, Stern RG, Cann CE, Herfkens RJ, Brundage BH. CT-determined pulmonary artery diameters in predicting pulmonary hypertension. Invest Radiol. 1984; 19:16–22.18. Ng CS, Wells AU, Padley SP. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging. 1999; 14:270–278.19. Mao SS, Ahmadi N, Shah B, Beckmann D, Chen A, Ngo L, Flores FR, Gao YL, Budoff MJ. Normal thoracic aorta diameter on cardiac computed tomography in healthy asymptomatic adults: impact of age and gender. Acad Radiol. 2008; 15:827–834.20. Wolak A, Gransar H, Thomson LE, Friedman JD, Hachamovitch R, Gutstein A, Shaw LJ, Polk D, Wong ND, Saouaf R, et al. Aortic size assessment by noncontrast cardiac computed tomography: normal limits by age, gender, and body surface area. JACC Cardiovasc Imaging. 2008; 1:200–209.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Significances of Bronchial Anthracofibrosis in the Patients with Endobronchial Tuberculosis
- A Case of Extrinsic Compression of the Left Main Coronary Artery Secondary to Pulmonary Artery Dilatation
- Aneurysm of the Main Pulmonary Artery-Report of a case and review of the literature
- Pulmonary Vein Varix: A Case Report
- A Case of Asymptomatic Patient with Idiopathic Pulmonary Artery Aneurysm