J Korean Med Sci.
2014 Sep;29(Suppl 2):S103-S108. 10.3346/jkms.2014.29.S2.S103.
A Higher Salt Intake Leads to a Lower Rate of Adequate Blood Pressure Control
- Affiliations
-
- 1Department of Internal Medicine, Hallym University Hangang Sacred Heart Hospital, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 3Nephrology Clinic, National Cancer Center, Goyang, Korea.
- 4Department of Internal Medicine, Konkuk University School of Medicine, Chungju, Korea.
- 5Research Institute of Salt and Health, Seoul K-Clinic, Seoul, Korea.
- 6Department of Internal Medicine, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea. jieunmd@gmail.com
- KMID: 2069800
- DOI: http://doi.org/10.3346/jkms.2014.29.S2.S103
Abstract
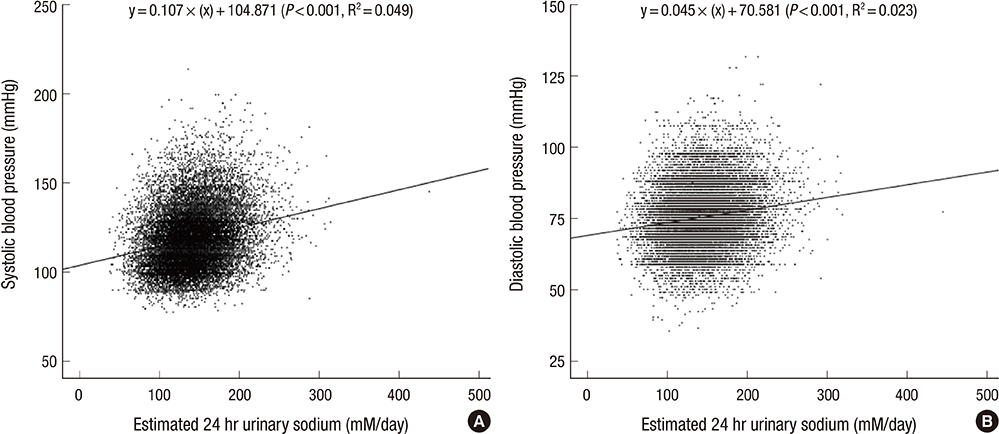
- The relationship between salt intake and adequate blood pressure control is not well investigated in Korea populations, especially in patients with cardiovascular disease. This cross-sectional study enrolled 19,083 subjects who participated in the Korea National Health and Nutrition Examination Survey conducted from 2009-2011. The amount of salt intake was estimated using the Tanaka equations based on spot urine samples. Comparing patients with and without cardiovascular disease, systolic blood pressure (129.1+/-18.1 mmHg vs. 120.0+/-18.1 mmHg, P<0.001) and the amount of urinary sodium excretion (149.4+/-37.5 mM/day vs. 144.1+/-36.2 mM/day, P<0.001) were higher in patients with cardiovascular diseases. Among patients with cardiovascular disease, the high blood pressure group showed an increased amount of urinary sodium excretion compared to the normal blood pressure group (155.5+/-38.2 vs. 146.6+/-36.9 mM/day, P<0.001). The odds ratio (OR) of high blood pressure was higher (OR, 1.825; 95% CI, 1.187-2.807; P-for-trend 0.003, highest quartile of urinary sodium excretion vs. lowest quartile) in patients with cardiovascular disease. A higher amount of urinary sodium excretion was associated with a lower rate of adequate blood pressure control in Korean population, especially with cardiovascular disease.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effects of interaction between SLC12A3 polymorphism, salt-sensitive gene, and sodium intake on risk of child obesity
∗
Joohyun Jung, Myoungsook Lee
J Nutr Health. 2017;50(1):32-40. doi: 10.4163/jnh.2017.50.1.32.
Reference
-
1. Elliott P, Walker LL, Little MP, Blair-West JR, Shade RE, Lee DR, Rouquet P, Leroy E, Jeunemaitre X, Ardaillou R, et al. Change in salt intake affects blood pressure of chimpanzees: implications for human populations. Circulation. 2007; 116:1563–1568.2. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hr urinary sodium and potassium excretion. BMJ. 1988; 297:319–328.3. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002; 360:1903–1913.4. Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011; 377:1438–1447.5. World Health Organization. Guideline: Sodium intake for adults and children. Geneva: World Health Organization;2012.6. McGuire S. U.S. Department of Agriculture and U.S. Department of Health and Human Services, Dietary Guidelines for Americans, 2010. 7th ed. Washington DC: U.S. Government Printing Office, January 2011. Adv Nutr. 2011; 2:293–294.7. He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet. 2011; 378:380–382.8. US Department of Health and Human Services. Dietary guidelines for Americans 2010. US Department of Agriculture. 7th ed. Washington DC: US Government Printing Office;2010.9. Korea Centers for Disease Control and Prevention. The forth Korea National Health and Nutrition Examination Survey (KNHANES IV-3): Korea Health Statistics. 2009.10. Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T. A simple method to estimate populational 24-hr urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002; 16:97–103.11. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001; 344:3–10.12. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA. 1996; 275:1571–1576.13. Lawes CM, Rodgers A, Bennett DA, Parag V, Suh I, Ueshima H, MacMahon S. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003; 21:707–716.14. He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010; 52:363–382.15. He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2013; 4:CD004937.16. Zhou B, Wang HL, Wang WL, Wu XM, Fu LY, Shi JP. Long-term effects of salt substitution on blood pressure in a rural north Chinese population. J Hum Hypertens. 2013; 27:427–433.17. Holbrook JT, Patterson KY, Bodner JE, Douglas LW, Veillon C, Kelsay JL, Mertz W, Smith JC Jr. Sodium and potassium intake and balance in adults consuming self-selected diets. Am J Clin Nutr. 1984; 40:786–793.18. Tsuchihashi T, Kai H, Kusaka M, Kawamura M, Matsuura H, Miura K, Ando K, Maruyama S, Hayabuchi H, Takagi Y, et al. [Scientific statement] Report of the Salt Reduction Committee of the Japanese Society of Hypertension (3) Assessment and application of salt intake in the management of hypertension. Hypertens Res. 2013; 36:1026–1031.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dietary Salt and Potassium Intake and Hypertension
- Time-Related Alterations of Endogenous Ouabain in DOCA-Salt Hypertensive Rats
- Dietary Salt Intake and Hypertension
- Effects of mineral-rich salt intake on the serum and blood pressure of Dahl salt-sensitive rats
- Plasma Renin Activity on Postural Change and Blood Sodium in Essential Hypertension