Pediatr Gastroenterol Hepatol Nutr.
2015 Sep;18(3):180-186. 10.5223/pghn.2015.18.3.180.
Asymptomatic Bile Duct Dilatation in Children: Is It a Disease?
- Affiliations
-
- 1Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. pedks@yuhs.ac
- 2Department of Radiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2068795
- DOI: http://doi.org/10.5223/pghn.2015.18.3.180
Abstract
- PURPOSE
Bile duct dilatation is a relatively common sonographic finding; nevertheless, its clinical significance in children is controversial because little research has been done in the area. Therefore, we investigated the natural course and clinical significance of biliary duct dilatation in children.
METHODS
We performed a retrospective study of 181 children (range, 1-day-old to 17-year-old) in whom dilatation of the intrahepatic duct and/or common hepatic duct and/or common bile duct was detected by abdominal ultrasonography at the Severance Children's Hospital between November 2005 and March 2014. We reviewed and analyzed laboratory test results, clinical manifestations, and clinical course in these patients.
RESULTS
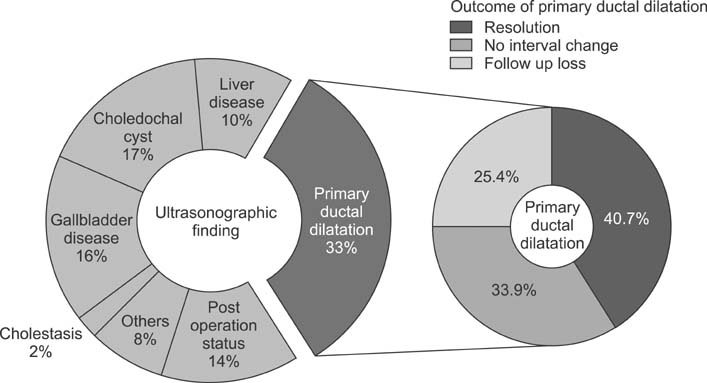
Pediatric patients (n=181) were enrolled in the study and divided into two groups. The first group included 59 subjects, without definitive cause of bile duct dilatation, who did not require treatment; the second group included 122 subjects, with definitive cause of bile duct dilatation or underlying biliary disease, who did require treatment. In the first group, 24 patients (40.7%) showed spontaneous resolution of bile duct dilatation, 20 patients (33.9%) showed no change, and 15 patients (25.4%) were lost to follow-up. In the second group, 31 patients were diagnosed with choledochal cysts, and 91 patients presented with biliary tract dilatations due to secondary causes, such as gallbladder or liver disease, post-operative complications, or malignancy.
CONCLUSION
Biliary dilatation in pediatric patients without symptoms, and without laboratory and other sonographic abnormalities, showed a benign clinical course. No pathologic conditions were noted on follow-up ultrasonography.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Management of Pediatric Patients Presenting with Acute Abdomen Accompanying Dilatation of the Common Bile Duct
Young A Kim, Gyung Min Kim, Peter Chun, Eun Ha Hwang, Sang Wook Mun, Yeoun Joo Lee, Jae Hong Park
Pediatr Gastroenterol Hepatol Nutr. 2018;21(3):203-208. doi: 10.5223/pghn.2018.21.3.203.
Reference
-
1. Gore RM, Levine MS. Textbook of gastrointestinal radiology. Philadelphia: Elsevier;2015.2. Brant WE, Helms CA. Fundamentals of diagnostic radiology. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health;2012.3. Bowie JD. What is the upper limit of normal for the common bile duct on ultrasound: how much do you want it to be? Am J Gastroenterol. 2000; 95:897–900.
Article4. Oppong KW, Mitra V, Scott J, Anderson K, Charnley RM, Bonnington S, et al. Endoscopic ultrasound in patients with normal liver blood tests and unexplained dilatation of common bile duct and or pancreatic duct. Scand J Gastroenterol. 2014; 49:473–480.
Article5. Bruno M, Brizzi RF, Mezzabotta L, Carucci P, Elia C, Gaia S, et al. Unexplained common bile duct dilatation with normal serum liver enzymes: diagnostic yield of endoscopic ultrasound and follow-up of this condition. J Clin Gastroenterol. 2014; 48:e67–e70.6. Jeon J, Song SY, Lee KT, Lee KH, Bae MH, Lee JK. Clinical significance and long-term outcome of incidentally found bile duct dilatation. Dig Dis Sci. 2013; 58:3293–3299.
Article7. Lin SF, Lee HC, Yeung CY, Jiang CB, Chan WT. Common bile duct dilatations in asymptomatic neonates: incidence and prognosis. Gastroenterol Res Pract. 2014; 2014:392562.
Article8. Gan SI, Rajan E, Adler DG, Baron TH, Anderson MA, Cash BD, et al. ASGE Standards of Practice Committee. Role of EUS. Gastrointest Endosc. 2007; 66:425–434.
Article9. Fernández-Esparrach G, Ginès A, Sánchez M, Pagés M, Pellisé M, Fernández-Cruz L, et al. Comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the diagnosis of pancreatobiliary diseases: a prospective study. Am J Gastroenterol. 2007; 102:1632–1639.
Article10. Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL. Choledochal cyst disease. A changing pattern of presentation. Ann Surg. 1994; 220:644–652.
Article11. Park HJ, Shin CG, Moon JS, Lee CG. Analysis of hepatobiliary disorders from a nationwide survey ofdischarge data in Korean children and adolescents. Korean J Pediatr Gastroenterol Nutr. 2009; 12:16–22.
Article12. Zhang Y, Wang XL, Li SX, Bai YZ, Ren WD, Xie LM, et al. Ultrasonographic dimensions of the common bile duct in Chinese children: results of 343 cases. J Pediatr Surg. 2013; 48:1892–1896.
Article13. Douillet P, Brunelle F, Chaumont P, Valayer J, Sassoon C, Odièvre M. Ultrasonography and percutaneous cholangiography in children with dilated bile ducts. Report of six cases. Am J Dis Child. 1981; 135:131–133.
Article14. Arima E, Akita H. Congenital biliary tract dilatation and anomalous junction of the pancreatico-biliary ductal system. J Pediatr Surg. 1979; 14:9–15.
Article15. Büyükyavuz I, Karnak I, Haliloglu M, Senocak ME. Inflammatory myofibroblastic tumour of the extrahepatic bile ducts: an unusual cause of obstructive jaundice in children. Eur J Pediatr Surg. 2003; 13:421–424.
Article16. Tas A, Koklu S. Unusual cause of common bile duct dilatation in asymptomatic elderly patient: right hepatic artery syndrome. Ann Hepatol. 2012; 11:150–151.
Article17. Tahara K, Ishimaru Y, Fujino J, Suzuki M, Hatanaka M, Igarashi A, et al. Association of extrahepatic bile duct duplication with pancreaticobiliary maljunction and congenital biliary dilatation in children: a case report and literature review. Surg Today. 2013; 43:800–805.
Article18. McGahan JP, Phillips HE, Cox KL. Sonography of the normal pediatric gallbladder and biliary tract. Radiology. 1982; 144:873–875.
Article19. Hernanz-Schulman M, Ambrosino MM, Freeman PC, Quinn CB. Common bile duct in children: sonographic dimensions. Radiology. 1995; 195:193–195.
Article20. Siegel MJ. Liver and biliary tract. In : Siegel MJ, editor. Pediatric sonography. 2nd ed. New York: Raven Press;1995. p. 171.21. Naji O, Hussain A, Baker D, Habib N, El-Hasani S. Obstructive jaundice due to autoimmune cholangiopathy. BMJ Case Rep. 2009; 2009.
Article22. Fumino S, Iwai N, Deguchi E, Shimadera S, Iwabuchi T, Nishimura T, et al. Bleeding tendency as a first symptom in children with congenital biliary dilatation. Eur J Pediatr Surg. 2007; 17:2–5.
Article23. Riederer J. Obstructive jaundice du to sludge in the common bile duct. Dtsch Med Wochenschr. 2000; 125:11–14.24. Senturk S, Miroglu TC, Bilici A, Gumus H, Tekin RC, Ekici F, et al. Diameters of the common bile duct in adults and postcholecystectomy patients: a study with 64-slice CT. Eur J Radiol. 2012; 81:39–42.
Article25. Landry D, Tang A, Murphy-Lavallée J, Lepanto L, Billiard JS, Olivié D, et al. Dilatation of the bile duct in patients after cholecystectomy: a retrospective study. Can Assoc Radiol J. 2014; 65:29–34.
Article26. Daradkeh S, Tarawneh E, Al-Hadidy A. Factors affecting common bile duct diameter. Hepatogastroenterology. 2005; 52:1659–1661.27. Lee HC, Yeung CY, Chang PY, Sheu JC, Wang NL. Dilatation of the biliary tree in children: sonographic diagnosis and its clinical significance. J Ultrasound Med. 2000; 19:177–182. quiz 183-4
Article28. Kim JE, Lee JK, Lee KT, Park DI, Hyun JG, Paik SW, et al. The clinical significance of common bile-duct dilatation in patients without biliary symptoms or causative lesions on ultrasonography. Endoscopy. 2001; 33:495–500.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Approach for Asymptomatic Bile Duct Dilatation
- A Common Bile Duct Web in Association with Bile Duct Stone Treated with Balloon Dilatation
- Solitary intrahepatic bile-duct cyst presenting with jaundice
- Transient common bile duct dilatation in infants
- Intrahepatic Bile Duct Dilatation Caused by Pancreatic Pseudocyst: A Case Report