Yonsei Med J.
2014 May;55(3):800-806. 10.3349/ymj.2014.55.3.800.
Finding the 'Ideal' Regimen for Fentanyl-Based Intravenous Patient-Controlled Analgesia: How to Give and What to Mix?
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Severance Hospital, Seoul, Korea. seaoyster@yuhs.ac
- 2Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2068694
- DOI: http://doi.org/10.3349/ymj.2014.55.3.800
Abstract
- PURPOSE
This analysis was done to investigate the optimal regimen for fentanyl-based intravenous patient-controlled analgesia (IV-PCA) by finding a safe and effective background infusion rate and assessing the effect of adding adjuvant drugs to the PCA regimen.
MATERIALS AND METHODS
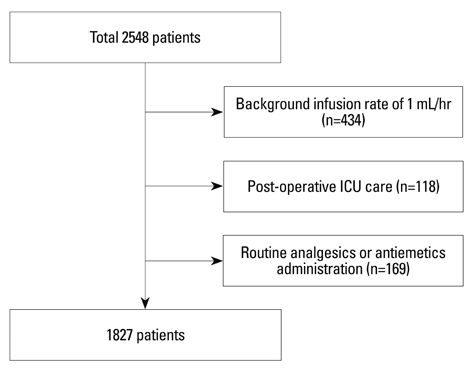
Background infusion rate of fentanyl, type of adjuvant analgesic and/or antiemetic that was added to the IV-PCA, and patients that required rescue analgesics and/or antiemetics were retrospectively reviewed in 1827 patients who underwent laparoscopic abdominal surgery at a single tertiary hospital.
RESULTS
Upon multivariate analysis, lower background infusion rates, younger age, and IV-PCA without adjuvant analgesics were identified as independent risk factors of rescue analgesic administration. Higher background infusion rates, female gender, and IV-PCA without additional 5HT3 receptor blockers were identified as risk factors of rescue antiemetics administration. A background infusion rate of 0.38 microg/kg/hr [area under the curve (AUC) 0.638] or lower required rescue analgesics in general, whereas, addition of adjuvant analgesics decreased the rate to 0.37 microg/kg/hr (AUC 0.712) or lower. A background infusion rate of 0.36 microg/kg/hr (AUC 0.638) or higher was found to require rescue antiemetics in general, whereas, mixing antiemetics with IV-PCA increased the rate to 0.37 microg/kg/hr (AUC 0.651) or higher.
CONCLUSION
Background infusion rates of fentanyl between 0.12 and 0.67 microg/kg/hr may safely be used without any serious side effects for IV-PCA. In order to approach the most reasonable background infusion rate for effective analgesia without increasing postoperative nausea and vomiting, adding an adjuvant analgesic and an antiemetic should always be considered.
MeSH Terms
Figure
Cited by 2 articles
-
The evaluation of implementing smart patient controlled analgesic pump with a different infusion rate for different time duration on postoperative pain management
Saeyoung Kim, Younghoon Jeon, Hyeonjun Lee, Jung A Lim, Sungsik Park, Si Oh Kim
J Dent Anesth Pain Med. 2016;16(4):289-294. doi: 10.17245/jdapm.2016.16.4.289.The efficacy of ultrasound-guided erector spinae plane block after mastectomy and immediate breast reconstruction with a tissue expander: a randomized clinical trial
Sukhee Park, Joohyun Park, Ji Won Choi, Yu Jeong Bang, Eun Jung Oh, Jiyeon Park, Kwan Young Hong, Woo Seog Sim
Korean J Pain. 2021;34(1):106-114. doi: 10.3344/kjp.2021.34.1.106.
Reference
-
1. Palmer PP, Miller RD. Current and developing methods of patient-controlled analgesia. Anesthesiol Clin. 2010; 28:587–599.
Article2. Ballantyne JC, Carr DB, Chalmers TC, Dear KB, Angelillo IF, Mosteller F. Postoperative patient-controlled analgesia: meta-analyses of initial randomized control trials. J Clin Anesth. 1993; 5:182–193.
Article3. Walder B, Schafer M, Henzi I, Tramèr MR. Efficacy and safety of patient-controlled opioid analgesia for acute postoperative pain. A quantitative systematic review. Acta Anaesthesiol Scand. 2001; 45:795–804.4. Momeni M, Crucitti M, De Kock M. Patient-controlled analgesia in the management of postoperative pain. Drugs. 2006; 66:2321–2337.
Article5. Kim SH, Shin YS, Oh YJ, Lee JR, Chung SC, Choi YS. Risk assessment of postoperative nausea and vomiting in the intravenous patient-controlled analgesia environment: predictive values of the Apfel's simplified risk score for identification of high-risk patients. Yonsei Med J. 2013; 54:1273–1281.
Article6. Grass JA. Patient-controlled analgesia. Anesth Analg. 2005; 101:5 Suppl. S44–S61.
Article7. Pasero C. Assessment of sedation during opioid administration for pain management. J Perianesth Nurs. 2009; 24:186–190.
Article8. Macintyre PE. Safety and efficacy of patient-controlled analgesia. Br J Anaesth. 2001; 87:36–46.
Article9. White I, Ghinea R, Avital S, Chazan S, Dolkart O, Weinbroum AA. Morphine at "sub-analgesic" background infusion rate plus low-dose PCA bolus control pain better and is as safe as twice a bolus-only PCA regimen: a randomized, double blind study. Pharmacol Res. 2012; 66:185–191.
Article10. Guler T, Unlugenc H, Gundogan Z, Ozalevli M, Balcioglu O, Topcuoglu MS. A background infusion of morphine enhances patient-controlled analgesia after cardiac surgery. Can J Anaesth. 2004; 51:718–722.
Article11. White PF, Kehlet H. Improving postoperative pain management: what are the unresolved issues? Anesthesiology. 2010; 112:220–225.12. Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet. 2011; 377:2215–2225.
Article13. Fleming BM, Coombs DW. A survey of complications documented in a quality-control analysis of patient-controlled analgesia in the postoperative patient. J Pain Symptom Manage. 1992; 7:463–469.
Article14. Sidebotham D, Dijkhuizen MR, Schug SA. The safety and utilization of patient-controlled analgesia. J Pain Symptom Manage. 1997; 14:202–209.
Article15. Schug SA, Torrie JJ. Safety assessment of postoperative pain management by an acute pain service. Pain. 1993; 55:387–391.
Article16. Hagle ME, Lehr VT, Brubakken K, Shippee A. Respiratory depression in adult patients with intravenous patient-controlled analgesia. Orthop Nurs. 2004; 23:18–27.
Article17. Pasero C, McCaffery M. Safe use of a continuous infusion with i.v. PCA. J Perianesth Nurs. 2004; 19:42–45.
Article18. Sam WJ, MacKey SC, Lötsch J, Drover DR. Morphine and its metabolites after patient-controlled analgesia: considerations for respiratory depression. J Clin Anesth. 2011; 23:102–106.
Article19. Mather LE. Opioids: a pharmacologist's delight! Clin Exp Pharmacol Physiol. 1995; 22:833–836.
Article20. Cepeda MS, Farrar JT, Baumgarten M, Boston R, Carr DB, Strom BL. Side effects of opioids during short-term administration: effect of age, gender, and race. Clin Pharmacol Ther. 2003; 74:102–112.
Article21. Hutchison RW, Chon EH, Tucker JW, Gilder R, Moss J, Daniel P. A Comparison of a Fentanyl, Morphine, and Hydromorphone Patient-Controlled Intravenous Delivery for Acute Postoperative Analgesia: A Multicenter Study of Opioid-Induced Adverse Reactions. Hosp Pharm. 2006; 41:659–663.
Article22. Kim SY, Kim EM, Nam KH, Chang DJ, Nam SH, Kim KJ. Postoperative intravenous patient-controlled analgesia in thyroid surgery: comparison of fentanyl and ondansetron regimens with and without the nonsteriodal anti-inflammatory drug ketorolac. Thyroid. 2008; 18:1285–1290.
Article23. Song JW, Park EY, Lee JG, Park YS, Kang BC, Shim YH. The effect of combining dexamethasone with ondansetron for nausea and vomiting associated with fentanyl-based intravenous patient-controlled analgesia. Anaesthesia. 2011; 66:263–267.
Article24. Lui F, Ng KF. Adjuvant analgesics in acute pain. Expert Opin Pharmacother. 2011; 12:363–385.
Article25. Fletcher D, Fermanian C, Mardaye A, Aegerter P. Pain and Regional Anesthesia Committee of the French Anesthesia and Intensive Care Society (SFAR). A patient-based national survey on postoperative pain management in France reveals significant achievements and persistent challenges. Pain. 2008; 137:441–451.
Article26. Kehlet H, Dahl JB. The value of "multimodal" or "balanced analgesia" in postoperative pain treatment. Anesth Analg. 1993; 77:1048–1056.
Article27. Kehlet H, Werner M, Perkins F. Balanced analgesia: what is it and what are its advantages in postoperative pain? Drugs. 1999; 58:793–797.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The efficacy of the time-scheduled decremental continuous infusion of fentanyl for postoperative patient-controlled analgesia after total intravenous anesthesia
- Comparison of the Effects of Postoperative Continuous Plus Bolus Patient-Controlled Analgesia and of Bolus Patient-Controlled Analgesia in Children
- Intravenous Patient-controlled Analgesia for Postoperative Pain Management in Patients with Cerebral Palsy
- Is a Basal Infusion Required in Patient-controlled Analgesia Using Fentanyl after Orthopedic Surgery?
- The Analgesic Efficacy of Transdermal Fentanyl Patch with Intravenous Ketorolac by Patient Controlled Analgesia after Total Abdominal Hysterectomy