J Korean Neurosurg Soc.
2014 Jul;56(1):5-10. 10.3340/jkns.2014.56.1.5.
Feasibility of Bilateral Crossing C7 Intralaminar Screws: A Cadaveric Study
- Affiliations
-
- 1Department of Neurosurgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea. nsman72@hanmail.net
- 2Department of Neurosurgery, Memorial Hermann Hospital, University of Texas Health Science Center at Houston, Houston, TX, USA.
- KMID: 2067069
- DOI: http://doi.org/10.3340/jkns.2014.56.1.5
Abstract
OBJECTIVE
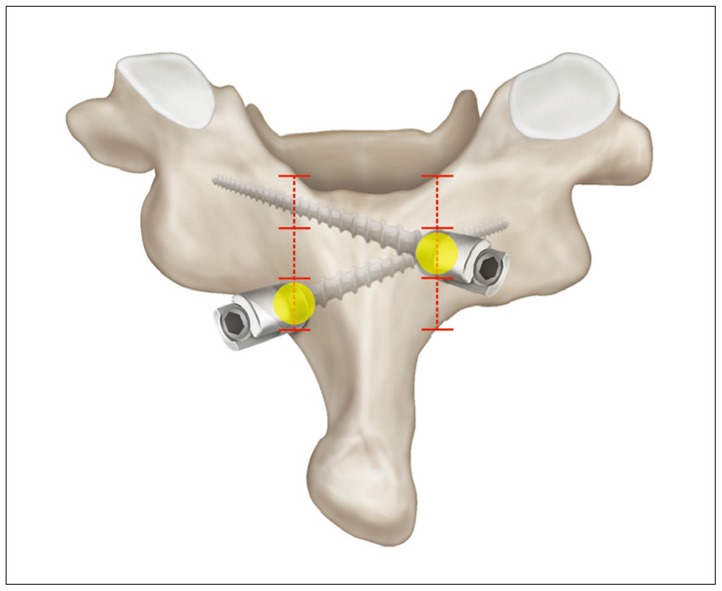
When the pedicle screw insertion technique is failed or not applicable, C7 intralaminar screw insertion method has been used as an alternative or salvage fixation method recently. However, profound understanding of anatomy is required for safe application of the bilaterally crossing laminar screw at C7 in clinic. In this cadaveric study, we evaluated the anatomic feasibility of the bilateral crossing intralaminar screw insertion and especially focused on determination of proper screw entry point.
METHODS
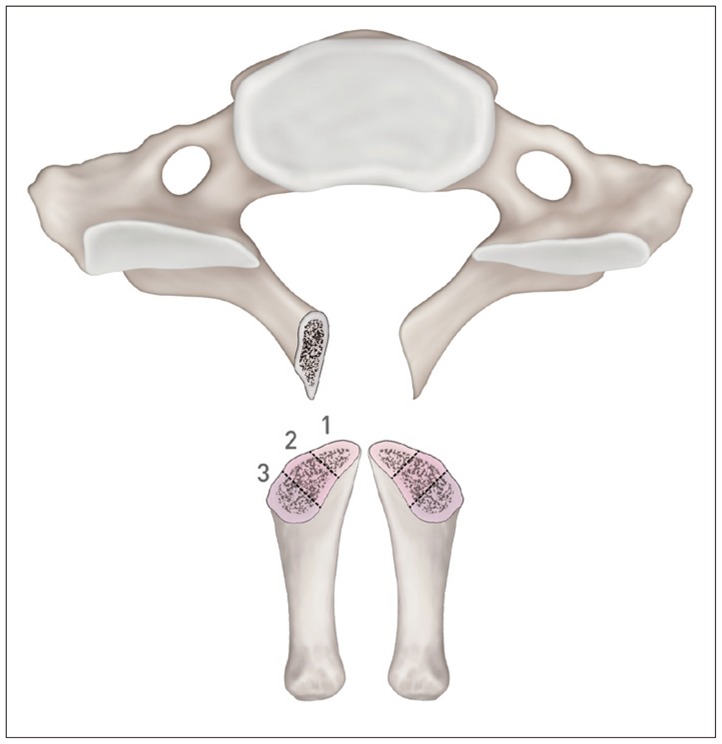
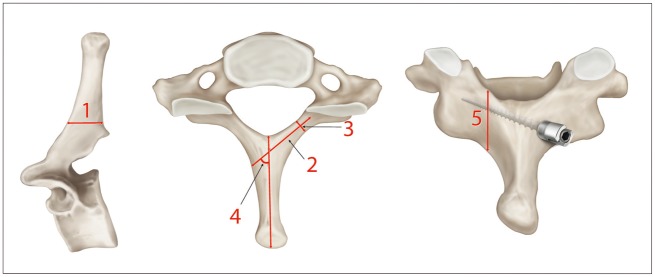
The C7 vertebrae from 18 adult specimens were studied. Morphometric measurements of the mid-laminar height, the minimum laminar thickness, the maximal screw length, and spino-laminar angle were performed and cross-sectioned vertically at the screw entry point (spino-laminar junction). The sectioned surface was equally divided into 3 parts and maximal thickness and surface area of the parts were measured. All measurements were obtained bilaterally.
RESULTS
The mean mid-laminar height was 13.7 mm, mean minimal laminar thickness was 6.6 mm, mean maximal screw length was 24.6 mm, and mean spinolaminar angle was 50.8+/-4.7degrees. Based on the measured laminar thickness, the feasibility of 3.5 mm diameter intralaminar screw application was 83.3% (30 sides laminae out of total 36) when assuming a tolerance of 1 mm on each side. Cross-sectional measurement results showed that the mean maximal thickness of upper, middle, and lower thirds was 5.0 mm, 7.5 mm, and 7.3 mm, respectively, and mean surface area for each part was 21.2 mm2, 46.8 mm2, and 34.7 mm2, respectively. Fourteen (38.9%) sides of laminae would be feasible for 3.5 mm intralaminar screw insertion when upper thirds of C7 spino-laminar junction is the screw entry point. In case of middle and lower thirds of C7 spino-laminar junction, 32 (88.9%) and 28 (77.8%) sides of laminae were feasible for 3.5 mm screw insertion, respectively.
CONCLUSION
The vertical cross-sectioned area of middle thirds at C7 spinolaminar junction was the largest area and 3.5 mm screw can be accommodated with 77.8% of feasibility when lower thirds were the screw entry point. Thus, selection of middle and lower thirds for each side of screw entry point in spino-laminar junction would be the safest way to place bilateral crossing laminar screw within the entire lamina. This anatomic study result will help surgeons to place the screw safely and accurately.
Keyword
Figure
Reference
-
1. Abumi K, Itoh H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine : description of the techniques and preliminary report. J Spinal Disord. 1994; 7:19–28. PMID: 8186585.
Article2. An HS, Gordin R, Renner K. Anatomic considerations for plate-screw fixation of the cervical spine. Spine (Phila Pa 1976). 1991; 16(10 Suppl):S548–S551. PMID: 1801270.
Article3. Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VK, Papadopoulos SM, et al. Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine (Phila Pa 1976). 2005; 30:915–922. PMID: 15834336.
Article4. Harris BM, Hilibrand AS, Nien YH, Nachwalter R, Vaccaro A, Albert TJ, et al. A comparison of three screw types for unicortical fixation in the lateral mass of the cervical spine. Spine (Phila Pa 1976). 2001; 26:2427–2431. PMID: 11707704.
Article5. Hong JT, Sung JH, Son BC, Lee SW, Park CK. Significance of laminar screw fixation in the subaxial cervical spine. Spine (Phila Pa 1976). 2008; 33:1739–1743. PMID: 18628706.
Article6. Hong JT, Tomoyuki T, Udayakumar R, Espinoza Orías AA, Inoue N, An HS. Biomechanical comparison of three different types of C7 fixation techniques. Spine (Phila Pa 1976). 2011; 36:393–398. PMID: 21325933.
Article7. Hong JT, Yi JS, Kim JT, Ji C, Ryu KS, Park CK. Clinical and radiologic outcome of laminar screw at C2 and C7 for posterior instrumentation--review of 25 cases and comparison of C2 and C7 intralaminar screw fixation. World Neurosurg. 2010; 73:112–118. discussion e15. PMID: 20860937.
Article8. Jang WY, Kim IS, Lee HJ, Sung JH, Lee SW, Hong JT. A computed tomography-based anatomic comparison of three different types of c7 posterior fixation techniques : pedicle, intralaminar, and lateral mass screws. J Korean Neurosurg Soc. 2011; 50:166–172. PMID: 22102943.
Article9. Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ. Transpedicle screw fixation of the cervical spine. Clin Orthop Relat Res. 1999; 359:77–88. PMID: 10078131.
Article10. Ma XY, Yin QS, Wu ZH, Xia H, Riew KD, Liu JF. C2 anatomy and dimensions relative to translaminar screw placement in an Asian population. Spine (Phila Pa 1976). 2010; 35:704–708. PMID: 20195212.
Article11. Şenoğlu M, Özkan F, Çelik M. Placement of C-7 intralaminar screws : a quantitative anatomical and morphometric evaluation. J Neurosurg Spine. 2012; 16:509–512. PMID: 22339053.
Article12. Wang MY. C2 crossing laminar screws : cadaveric morphometric analysis. Neurosurgery. 2006; 59(1 Suppl 1):ONS84–ONS88. discussion ONS84-ONS88. PMID: 16888557.13. Wang MY. Cervical crossing laminar screws : early clinical results and complications. Neurosurgery. 2007; 61(5 Suppl 2):311–315. discussion 315-316. PMID: 18091245.14. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws : case series and technical note. J Spinal Disord Tech. 2004; 17:158–162. PMID: 15260101.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- C7 Posterior Fixation Using Intralaminar Screws : Early Clinical and Radiographic Outcome
- The Feasibility of Translaminar Screws in the Subaxial Cervical Spine: Computed Tomography and Cadaveric Validation
- A Computed Tomography-Based Anatomic Comparison of Three Different Types of C7 Posterior Fixation Techniques : Pedicle, Intralaminar, and Lateral Mass Screws
- Comparison of Three Different Options for C7 Posterior Vertebral Anchor in the Indian Population—Lateral Mass, Pedicle, and Lamina: A Computed Tomography-Based Morphometric Analysis
- A Biomechanical Comparison of Intralaminar C7 Screw Constructs with and without Offset Connector Used for C6-7 Cervical Spine Immobilization : A Finite Element Study