J Korean Med Assoc.
2006 Oct;49(10):939-950. 10.5124/jkma.2006.49.10.939.
Surgical Management of Obstructed Defecation
- Affiliations
-
- 1Department of Surgery, Konkuk University College of Medicine, Korea. ungchaepark@dreamwiz.com
- KMID: 2064973
- DOI: http://doi.org/10.5124/jkma.2006.49.10.939
Abstract
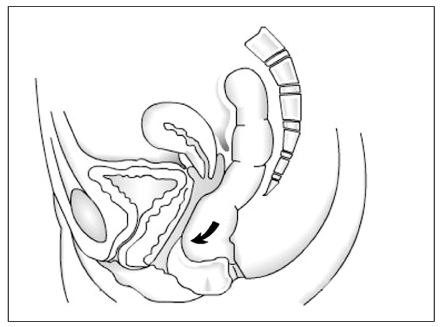
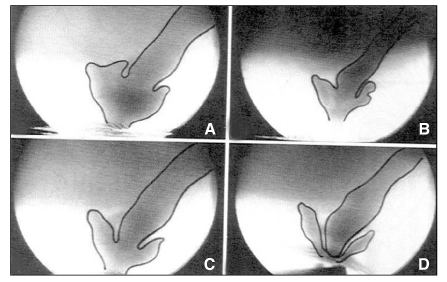
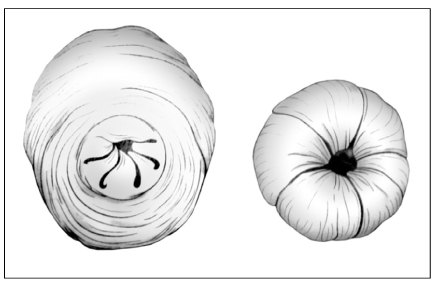
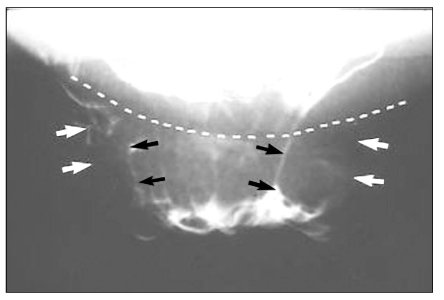
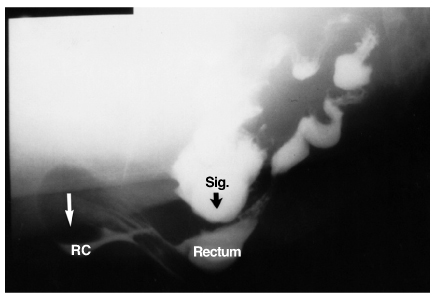
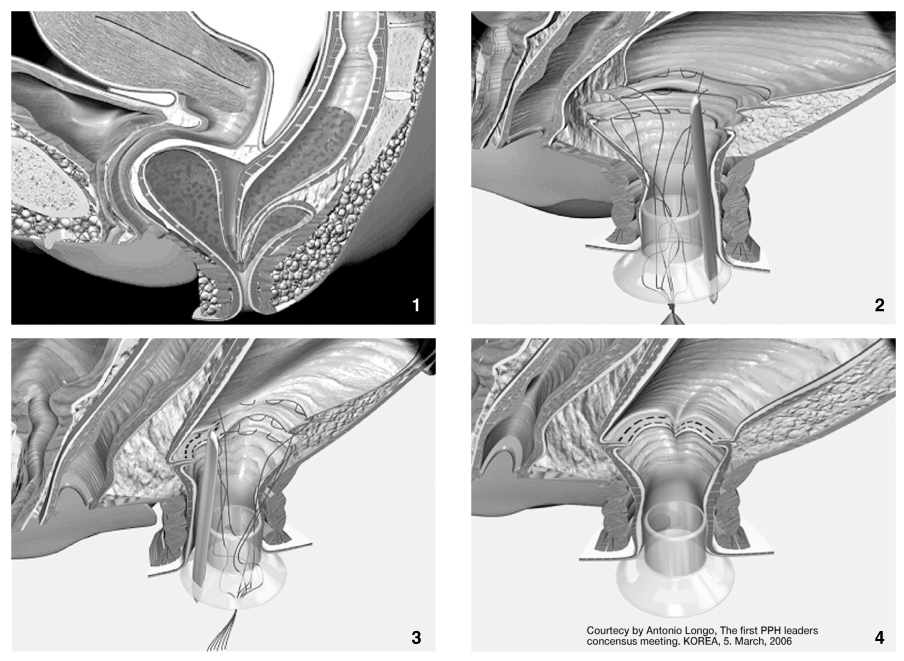
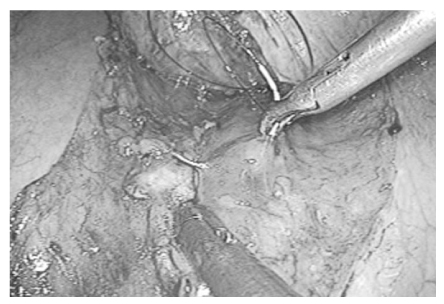
- There are three groups of patients with constipating symptoms; those with obstructed defecation, slow transit constipation, or both. The treatment of obstructed defecation (pelvic outlet obstruction) is often challenging because the underlying disorders are diverse with a wide range of and clinical symptoms. The underlying anatomical and pathophysiological changes in patients with obstructed defecation are complex and often poorly understood. As a consequence, many medical, surgical, and behavioral approaches have been described, with no single panacea. For successful outcomes, preoperative physiologic testing is mandatory to differentiate between obstructed defecation caused by pelvic outlet obstruction and slow transit constipation. Obstructed defecatory disorders can distress patients both socially and psychologically and greatly impair their quality of life. For the great majority of patients, dietary adjustment with an increased fiber and liquid supplement can resolve the symptoms. The surgical approach depends upon the etiology, severity of symptoms, and operative risks. In a small group of patients with a rectocele or a third degree sigmoidocele, surgical intervention yields a high success rate. Division or resection of the puborectalis muscle is not recommended. In patients with a mixed pattern of slow transit colon and pelvic outlet obstruction, surgical intervention alone is often not successful; these patients can experience better outcomes by conservative treatment of pelvic outlet obstruction, followed by a colectomy. Stapled transanal rectal resection has recently become a recommended surgical procedure for obstructed defecation syndrome. One problem when using a transanal stapling device for rectal surgery is the potential damage to the structures located in front of the anterior rectal wall. The laparoscopic approach can shorten the hospital stay with good outcomes and is well tolerated in elderly patients with rectal prolapse. Despite the progress in modern surgery, the choice of the surgical procedure of pelvic outlet obstruction is still controversial. Preoperative counseling of all patients undergoing surgery is of extreme importance, in particular to explain the evolving nature of pelvic floor dysfunction and the possible need for further reconstructive surgery. To identify patients who will benefit from surgery for obstructed defecation, a careful selection of candidate patients remains the crucial issue in the diagnostic assessment. Surgical intervention should be limited only to the patients with identifiable, surgically correctable causes of outlet obstruction. This review gives an overview of surgical treatment options in patients with obstructed defecation.
MeSH Terms
Figure
Reference
-
1. Lane WA. Result of the operative treatment of chronic constipation. BMJ. 1908. 1:1126–1130.2. Kuijpers JHC. Application of the colorectal laboratory in diagnosis and treatment of functional constipation. Dis Colon Rectum. 1990. 33:35–39.
Article3. Jo JS, Park UC. Diagnostic usefulness of anorectal physiologic investigation in patients with chronic constipation. Korean J Gastroenterol. 1998. 31:319–334.4. Ogunbiyi OA, Fleshman JW. Obstructed defecation: definitions and management options. Semin Colon Rectal Surg. 1996. 7:149–159.5. Park UC, Choi SK, Piccirillo MF, Verzaro R, Wexner SD. Patterns of anismus and the relation to biofeedback therapy. Dis Colon Rectum. 1996. 39:768.
Article6. Kim SK, Park UC. Rectocele : Anorectal physiologic characteristics and their clinical significances. J Korean Soc Coloproctol. 1996. 12:19–30.7. Karlbom U, Graf W, Nilsson S. Does surgical repair of a rectocele improve rectal emptying? Dis Colon Rectum. 1996. 39:1296–1302.
Article8. Christiansen J, Zhu BW, Rasmussen O, et al. Internal rectal intussusception: Result of surgical repair. Dis Colon Rectum. 1992. 35:1026–1029.9. Fleshman JW, Kodner IJ, Fry RD. Internal intussusception of the rectum: a changing perspective. Neth J Surg. 1989. 41:145–148.10. Jorge JMN, Yang YR, Wexner SD. Incidence and clinical significance of sigmoidoceles as determined by a new classification system. Dis Colon Rectum. 1994. 37:1112–1117.
Article11. Yoshioka K, Keighley MRB. Anorectal myectomy for outlet obstruction. Br J Surg. 1987. 74:373–376.
Article12. Yoshioka K, Keighley MRB. Randomized trial comparing anorectal myectomy and controlled anal dilatation for outlet obstruction. Br J Surg. 1987. 74:1125–1128.
Article13. Guillemot F, Leroi H, Lone YC, Rousseau CG, Lamblin MD, Cortot A. Action of in situ nitroglycerin on upper anal canal pressure of patients with terminal constipation: a pilot study. Dis Colon Rectum. 1993. 36:372–376.
Article14. Lubowski DZ, King DW. Obstructed defecation: current status of pathophysiology and management. Aust N Z J Surg. 1995. 65:87–92.
Article15. Park UC, Baik HK, Kim BG, Cho JS. Anal achalasia: Physiologic characteristics and their clinical significance. Collegium Internationale Chirurgiae Digestivae. 1996. 549.16. Park CJ. A clinical review of the rectocele. J Korean Soc Coloproctol. 1995. 11:115–121.17. Ommer A, Kohler A, Athanasiadis S. Results of transperineal levator-plasty in treatment of symptomatic rectocele. Chirurg. 1998. 09. 69:966–972.
Article18. Lechaux JP, Lechaux D, Bataille P, Bars I. Transperineal repair of rectocele with prosthetic mesh. A prospective study. Ann Chir. 2004. 129:211–217.19. Ayav A, Bresler L, Brunaud L, Boissel P. Long-term results of transanal repair of rectocele using linear stapler. Dis Colon Rectum. 2004. 47:889–894.
Article20. Altomare DF, Rinaldi M, Veglia A, Petrolino M, De Fazio M, Sallustio P. Combined perineal and endorectal repair of rectocele by circular stapler: a novel surgical technique. Dis Colon Rectum. 2002. 45:1549–1552.
Article21. Baessler K, Stanton SL. Sacrocolpopexy for vault prolapse and rectocele: do concomitant Burch colposuspension and perineal mesh detachment affect the outcome. Am J Obstet Gynecol. 2005. 192:1067–1072.
Article22. Petersen S, Hellmich G, Schuster A, Lehmann D, Albert W, Ludwig K. Stapled transanal rectal resection under laparoscopic surveillance for rectocele and concomitant enterocele. Dis Colon Rectum. 2006. 49:685–689.
Article23. Longo A. Stapled anopexy and stapled hemorrhoidectomy: two opposite concepts and procedures. Dis Colon Rectum. 2002. 45:571–572.
Article24. Pescatori M, Boffi F, Russo A, Zbar AP. Complications and recurrence after excision of rectal internal mucosal prolapse for obstructed defaecation. Int J Colorectal Dis. 2006. 21:160–165.
Article25. Tsiaoussis J, Chrysos E, Athanasakis E, Pechlivanides G, Tzortzinis A, Zoras O, Xynos E. Rectoanal intussusception: presentation of the disorder and late results of resection rectopexy. Dis Colon Rectum. 2005. 48:838–844.
Article26. Abbas SM, Bissett IP, Neill ME, Macmillan AK, Milne D, Parry BR. Long-term results of the anterior Delorme's operation in the management of symptomatic rectocele. Dis Colon Rectum. 2005. 48:317–322.
Article27. D'Hoore A, Cadoni R, Penninckx F. Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg. 2004. 91:1500–1505.28. Gadonneix P, Ercoli A, Salet-Lizee D, Cotelle O, Bolner B, Villet R, et al. Laparoscopic sacrocolpopexy with two separate meshes along the anterior and posterior vaginal walls for multicompartment pelvic organ prolapse. J Am Assoc Gynecol Laparosc. 2004. 11:29–35.
Article29. Fenner DE. Diagnosis and assessment of sigmoidoceles. Am J Obstet Gynecol. 1996. 175:1438–1441.
Article30. Farrell SA. Vaginal repair of a sigmoidocele. Int Urogynecol J Pelvic Floor Dysfunct. 2000. 11:325–327.
Article31. Martelli H, Devroede G, Arhan P, Duguay C. The mechanism of idiopathic constipation: outlet obstruction. Gastroenterology. 1978. 75:623–631.
Article32. Lysy J, Israeli E, Levy S, Rozentzweig G, Strauss-Liviatan N, Goldin E. Chemical sphincterotomy Long-Term Results of "Chemical Sphincterotomy" for Chronic Anal Fissure: A Prospective Study. Dis Colon Rectum. 2006. 06. 49:858–864.
Article33. Heymen S, Wexner SD, Gulledge AD. MMPI assessment of patients with functional bowel disorders. Dis Colon Rectum. 1993. 36:593–596.
Article34. Devroede G, Gilles G, Bouchoucha M, et al. Idiopathic constipation by colonic dysfunction: relationship with personality and anxiety. Dig Dis Sci. 1989. 34:1428–1433.35. Park UC, Yoo YB, Kim JJ, Nam BW. Psychiatric investigation by using the Minnesota multiphasic Personality Inventory in patients with chronic constipation. J Korean Soc Coloproctol. 2002. 18:95–103.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Management of Functional Evacuation Disorders
- Early Experience with a Stapled TransAnal Rectal Resection for Obstructed Defecation Syndrome
- Mucopexy-Recto Anal Lifting (MuRAL) in managing obstructed defecation syndrome associated with prolapsed hemorrhoids and rectocele: preliminary results
- Transmural Migration of Surgical Sponge Evacuated by Defecation: Mimicking an Intraperitoneal Gossypiboma
- A Case of Defecation-induced Epilepsy