Ann Surg Treat Res.
2020 May;98(5):277-282. 10.4174/astr.2020.98.5.277.
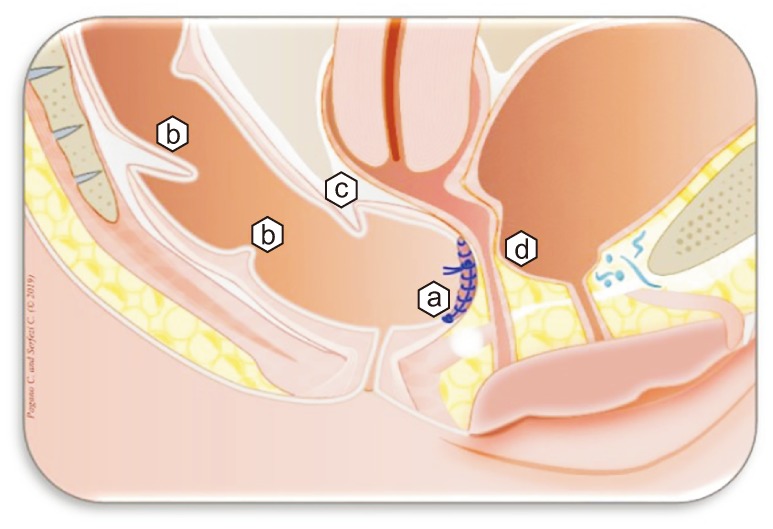
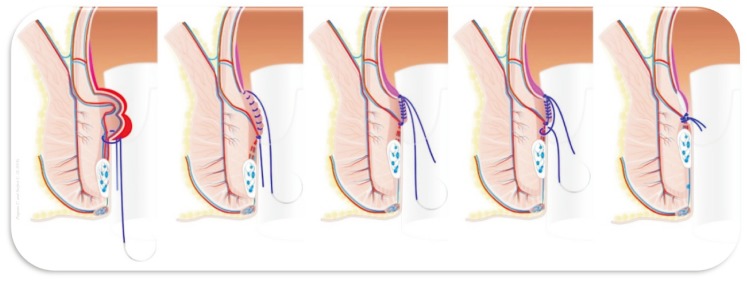
Mucopexy-Recto Anal Lifting (MuRAL) in managing obstructed defecation syndrome associated with prolapsed hemorrhoids and rectocele: preliminary results
- Affiliations
-
- 1General Surgery Unit, Vizzolo Predabissi Hospital, ASST Milano-Martesana, Vizzolo Predabissi (MI), Italy
- 2Day/Week Surgery Unit, Foundation IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy
- 3Department of Pathophysiology and Transplantation, University of Milano, Milan, Italy
- KMID: 2500829
- DOI: http://doi.org/10.4174/astr.2020.98.5.277
Abstract
- Purpose
Treatment of rectocele associated with prolapsed hemorrhoids is a debated topic. Transanal stapling achieved good midterm results in patients with symptoms of obstructed defecation, nevertheless a number of severe complications have been reported. The aim of this study was to evaluate the safety and efficacy of a new endorectal manual technique in patients with obstructed defecation due to the combination of muco-hemorrhoidal prolapse and rectocele.
Methods
Patients enrolled after preoperative obstructed defecation syndrome (ODS) score, defecography and anoscopy were submitted to the novel Mucopexy-Recto Anal Lifting (MuRAL) combined with a modified Block procedure, and followed up by independent observers with digital exploration 3 weeks postoperatively, and digital exploration plus anoscopy at 3, 6, and 12 months. Operative time, hospital stay, numerating rating scale (NRS), ODS, satisfaction scores, and recurrence rate were recorded.
Results
Mean operative time was 35.7 minutes. Fifty-six patients completed 1-year follow-up: 7.1% had acute urinary retention, NRS score was < 3 from the third postoperative day, mean time of daily activity resumption was 12 days, none had persistent fecal urgency, 82% declared excellent/good satisfaction score, significant improvement of 6- and 12-month ODS score, no recurrence of rectocele, and 7.1% recurrence of prolapsed hemorrhoids were observed.
Conclusion
MuRAL associated with modified Block technique gave no severe complications and resulted in a safe and effective approach to symptomatic rectocele associated with muco-rectal prolapse. Further randomized studies, larger series, and longer follow-up are needed.
Keyword
Figure
Reference
-
1. Boccasanta P, Venturi M, Calabro G, Trompetto M, Ganio E, Tessera G, et al. Which surgical approach for rectocele? A multicentric report from Italian coloproctologists. Tech Coloproctol. 2001; 5:149–156. PMID: 11875682.2. Block IR. Transrectal repair of rectocele using obliterative suture. Dis Colon Rectum. 1986; 29:707–711. PMID: 3533470.3. Tjandra JJ, Chan MK. Systematic review on the procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy). Dis Colon Rectum. 2007; 50:878–892. PMID: 17380367.4. Guttadauro A, Chiarelli M, Maternini M, Baini M, Pecora N, Gabrielli F. Value and limits of stapled transanal rectal repair for obstructed defecation syndrome: 10 years-experience with 450 cases. Asian J Surg. 2018; 41:573–577. PMID: 28693959.5. Pescatori M, Gagliardi G. Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech Coloproctol. 2008; 12:7–19. PMID: 18512007.6. Jayne DG, Schwandner O, Stuto A. Stapled transanal rectal resection for obstructed defecation syndrome: one-year results of the European STARR Registry. Dis Colon Rectum. 2009; 52:1205–1212. discussion 1212-4. PMID: 19571694.7. Pagano C, Vergani C, Invernizzi C, Bussone M, Benegiamo G, Venturi M. Mucopexyrecto anal lifting: a standardized minimally invasive method of managing symptomatic hemorrhoids, with an innovative suturing technique and the HemorPex System®. Minerva Chir. 2018; 73:469–474. PMID: 29652112.8. Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V. Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis. 2008; 10:84–88. PMID: 17441968.9. Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978; 37:378–381. PMID: 686873.10. Van Laarhoven CJ, Kamm MA, Bartram CI, Halligan S, Hawley PR, Phillips RK. Relationship between anatomic and symptomatic long-term results after rectocele repair for impaired defecation. Dis Colon Rectum. 1999; 42:204–210. discussion 210-1. PMID: 10211497.11. Sarles JC, Arnaud A, Selezneff I, Olivier S. Endo-rectal repair of rectocele. Int J Colorectal Dis. 1989; 4:167–171. PMID: 2768999.12. Cho SW, Lee RA, Chung SS, Kim KH. Early experience of doppler-guided hemorrhoidal artery ligation and rectoanal repair (DG-HAL & RAR) for the treatment of symptomatic hemorrhoids. J Korean Surg Soc. 2010; 78:23–28.13. Ratto C, Campenni P, Papeo F, Donisi L, Litta F, Parello A. Transanal hemorrhoidal dearterialization (THD) for hemorrhoidal disease: a single-center study on 1000 consecutive cases and a review of the literature. Tech Coloproctol. 2017; 21:953–962. PMID: 29170839.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transperineal rectocele repair is ideal for patients presenting with fecal incontinence
- Early postoperative outcomes of a novel nonexcisional technique using aluminum potassium sulfate and tannic acid sclerotherapy with mucopexy on patients with grade III hemorrhoids
- Pathogenesis and Surgical Treatment of Rectal Prolapse Syndrome
- Plication Method of the Redundant Rectal Mucosa by Longitudinal over and over Suture (overlaping suture)
- Adult Sigmoido-recto-anal Intussusception by a Sigmoid Colon Adenoma