J Gynecol Oncol.
2011 Sep;22(3):207-210. 10.3802/jgo.2011.22.3.207.
Pediatric vulvar squamous cell carcinoma in a liver transplantation recipient: a case report
- Affiliations
-
- 1Department of Pathology, Gil Medical Center, Incheon, Korea. hicho@gilhospital.com
- 2Department of Obstetrict and Gynecology, Gil Medical Center, Incheon, Korea.
- KMID: 2055710
- DOI: http://doi.org/10.3802/jgo.2011.22.3.207
Abstract
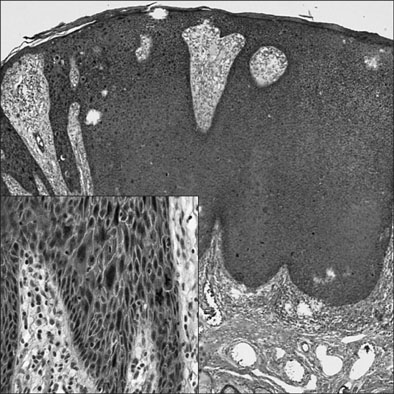
- Here we report the first Korean case of a girl who developed noninvasive squamous cell carcinoma of the vulva at the age of 16 years. She was taking tacrolimus, an immunosuppressive agent, after living-related liver transplantation. The vulvar masses were microscopically proved as vulvar intraepithelial neoplasm II and III, even squamous cell carcinoma in situ. Human papillomavirus subtypes (69 and 73) and human papillomavirus types (66, 70, 73, and 43) were detected in the vulvar mass and the cervicovaginal smear, respectively. The outcome of liver transplantation for children has been markedly improved during the last several decades. However, the present case highlights the need to perform periodic genital examinations for the adolescents after liver transplantation. In addition to the high risk and probable high subtypes, uncommonly found human papillomavirus subtypes were extracted from her vulvar cancer. The present case is the first to show the possible relationship between previously unknown and uncommon human papillomavirus subtypes and pediatric post-transplant vulvar squamous cell carcinoma. More attention should be paid to the vulvar and cervical surveillance of pediatric transplant recipients by both medical specialists and general physicians.
MeSH Terms
Figure
Reference
-
1. Koukourgianni F, Harambat J, Ranchin B, Euvrard S, Bouvier R, Liutkus A, et al. Malignancy incidence after renal transplantation in children: a 20-year single-centre experience. Nephrol Dial Transplant. 2010. 25:611–616.2. Kim KM. Current status of pediatric liver transplantation. Korean J Pediatr Gastroenterol Nutr. 2007. 10:1–10.3. Pagadala M, Dasarathy S, Eghtesad B, McCullough AJ. Posttransplant metabolic syndrome: an epidemic waiting to happen. Liver Transpl. 2009. 15:1662–1670.4. LaRosa C, Baluarte HJ, Meyers KE. Outcomes in pediatric solid-organ transplantation. Pediatr Transplant. 2011. 15:128–141.5. Hathout E, Alonso E, Anand R, Martz K, Imseis E, Johnston J, et al. Post-transplant diabetes mellitus in pediatric liver transplantation. Pediatr Transplant. 2009. 13:599–605.6. Penn I. De novo malignancy in pediatric organ transplant recipients. J Pediatr Surg. 1994. 29:221–226.7. Vajdic CM, McDonald SP, McCredie MR, van Leeuwen MT, Stewart JH, Law M, et al. Cancer incidence before and after kidney transplantation. JAMA. 2006. 296:2823–2831.8. Brown MR, Noffsinger A, First MR, Penn I, Husseinzadeh N. HPV subtype analysis in lower genital tract neoplasms of female renal transplant recipients. Gynecol Oncol. 2000. 79:220–224.9. Bosch FX, Lorincz A, Munoz N, Meijer CJ, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002. 55:244–265.10. de Villiers EM. Taxonomic classification of papillomaviruses. Papillomavirus Rep. 2001. 12:57–63.11. Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003. 348:518–527.12. Hong SR, Kim IS, Kim DW, Kim MJ, Kim AR, Kim YO, et al. Prevalence and genotype distribution of cervical human papillomavirus DNA in Korean women: a multicenter study. Korean J Pathol. 2009. 43:342–350.13. de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010. 11:1048–1056.14. Tedeschi SK, Savani BN, Jagasia M, Engelhardt B, Anasetti C, Barrett AJ, et al. Time to consider HPV vaccination after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2010. 16:1033–1036.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pregnancy following vulvar squamous cell carcinoma: a report of two cases
- Three Cases of Vulvar Squamous Cell Carcinoma Arising from Lichen Sclerosus
- A Case of Vulvar Carcinoma: Squamous Cell Carcinoma with Sarcomatoid Features
- A Case of Invasive Squamous Cell Carcinoma of the Vulva
- A Case of Squamous Cell Carcinoma of Gallbladder