Brain Tumor Res Treat.
2013 Oct;1(2):78-84. 10.14791/btrt.2013.1.2.78.
Treatment Options of Metastatic Brain Tumors from Hepatocellular Carcinoma: Surgical Resection vs. Gamma Knife Radiosurgery vs. Whole Brain Radiation Therapy
- Affiliations
-
- 1Department of Neurosurgery, Yonsei Gamma Knife Center, Yonsei University College of Medicine, Seoul, Korea. changws0716@yuhs.ac
- KMID: 2048479
- DOI: http://doi.org/10.14791/btrt.2013.1.2.78
Abstract
OBJECTIVE
Although metastasis of hepatocellular carcinoma to the brain is uncommon, it is associated with a very high mortality rate and most patients usually expire within 1 year after brain metastasis. The aim of this study is to identify the effectiveness of the active interventions such as gamma knife radiosurgery or surgical intervention for these patients.
METHODS
We retrospectively reviewed the medical records and imaging data of 59 patients with metastatic brain tumors from hepatocellular carcinoma from May 2004 to September 2012. The study included patients with available clinical and radiological data who had been diagnosed with metastatic hepatocellular carcinoma of the brain, confirmed by magnetic resonance imaging. The overall survival time was analyzed and compared according to each risk factor.
RESULTS
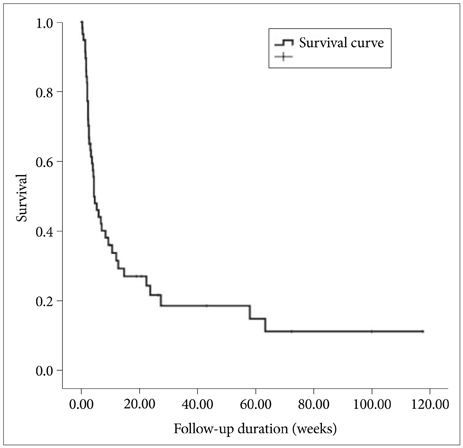
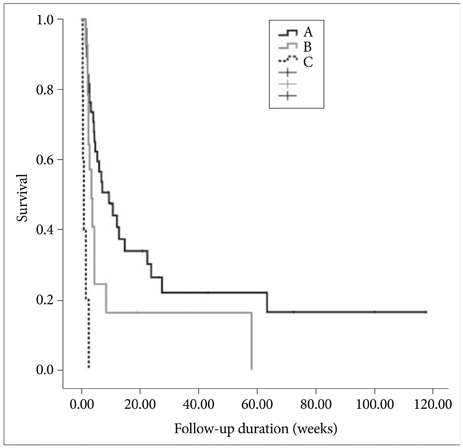
The mean age at diagnosis of metastatic brain tumor was 52.2 years (14-77). The mean follow-up duration was 13.3 weeks (0.1-117.6). Overall median survival was 4.3 weeks (95% confidence interval, 2.2-6.4). The results from an analysis of clinical factors related to survival revealed that treatment modalities were significantly related to the patient's survival (log rank, p=0.006). Twenty patients (32.8%) experienced tumor bleeding, and the survival time of the patients with tumor bleeding tended to be shorter, although the result was not statistically significant (log rank, p=0.058). Hepatic reserve, by Child-Pugh classification, was grade A in 38 patients (64.4%), grade B in 16 patients (27.1%), and grade C in 5 patients (8.5%), and was significantly related to the patient's survival (log rank, p=0.000).
CONCLUSION
Although patients with metastatic brain tumors from hepatocellular carcinoma showed poor survival, active intervention including surgical resection or gamma knife radiosurgery may result in better survival, especially if patients have preserved liver function.
MeSH Terms
Figure
Reference
-
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
Article2. Choi HJ, Cho BC, Sohn JH, et al. Brain metastases from hepatocellular carcinoma: prognostic factors and outcome: brain metastasis from HCC. J Neurooncol. 2009; 91:307–313.
Article3. Katyal S, Oliver JH 3rd, Peterson MS, Ferris JV, Carr BS, Baron RL. Extrahepatic metastases of hepatocellular carcinoma. Radiology. 2000; 216:698–703.
Article4. Kim M, Na DL, Park SH, Jeon BS, Roh JK. Nervous system involvement by metastatic hepatocellular carcinoma. J Neurooncol. 1998; 36:85–90.5. Murakami K, Nawano S, Moriyama N, et al. Intracranial metastases of hepatocellular carcinoma: CT and MRI. Neuroradiology. 1996; 38:Suppl 1. S31–S35.
Article6. Seinfeld J, Wagner AS, Kleinschmidt-DeMasters BK. Brain metastases from hepatocellular carcinoma in US patients. J Neurooncol. 2006; 76:93–98.
Article7. Carr BI. Hepatocellular carcinoma: current management and future trends. Gastroenterology. 2004; 127:5 Suppl 1. S218–S224.
Article8. Lai CR, Liu HC. Hepatocellular carcinoma in Taiwan: clinicopathological study of 440 cases from a consecutive 6000 autopsies. Zhonghua Yi Xue Za Zhi (Taipei). 1993; 51:249–256.9. Chang L, Chen YL, Kao MC. Intracranial metastasis of hepatocellular carcinoma: review of 45 cases. Surg Neurol. 2004; 62:172–177.
Article10. Chen SF, Tsai NW, Lui CC, et al. Hepatocellular carcinoma presenting as nervous system involvement. Eur J Neurol. 2007; 14:408–412.
Article11. Okuda K, Ohtsuki T, Obata H, et al. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients. Cancer. 1985; 56:918–928.
Article12. Arii S, Yamaoka Y, Futagawa S, et al. The Liver Cancer Study Group of Japan. Results of surgical and nonsurgical treatment for small-sized hepatocellular carcinomas: a retrospective and nationwide survey in Japan. Hepatology. 2000; 32:1224–1229.
Article13. Shiina S, Teratani T, Obi S, et al. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology. 2005; 129:122–130.
Article14. Shiina S, Tagawa K, Niwa Y, et al. Percutaneous ethanol injection therapy for hepatocellular carcinoma: results in 146 patients. AJR Am J Roentgenol. 1993; 160:1023–1028.
Article15. Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996; 334:693–699.
Article16. Llovet JM, Real MI, Montaña X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002; 359:1734–1739.
Article17. Kanda M, Tateishi R, Yoshida H, et al. Extrahepatic metastasis of hepatocellular carcinoma: incidence and risk factors. Liver Int. 2008; 28:1256–1263.
Article18. El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999; 340:745–750.
Article19. Yang WT, Yeo W, Leung SF, Chan YL, Johnson PJ, Metreweli C. MRI and CT of metastatic hepatocellular carcinoma causing spinal cord compression. Clin Radiol. 1997; 52:755–760.
Article20. Hsieh MJ, Lu CH, Tsai NW, et al. Prediction, clinical characteristics and prognosis of intracerebral hemorrhage in hepatocellular carcinoma patients with intracerebral metastasis. J Clin Neurosci. 2009; 16:394–398.
Article21. Jiang XB, Ke C, Zhang GH, et al. Brain metastases from hepatocellular carcinoma: clinical features and prognostic factors. BMC Cancer. 2012; 12:49.
Article22. Uchino K, Tateishi R, Shiina S, et al. Hepatocellular carcinoma with extrahepatic metastasis: clinical features and prognostic factors. Cancer. 2011; 117:4475–4483.
Article23. Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol. 2001; 2:533–543.
Article24. Chen PG, Lee SY, Barnett GH, et al. Use of the Radiation Therapy Oncology Group recursive partitioning analysis classification system and predictors of survival in 19 women with brain metastases from ovarian carcinoma. Cancer. 2005; 104:2174–2180.
Article25. Chang WS, Kim HY, Chang JW, Park YG, Chang JH. Analysis of radiosurgical results in patients with brain metastases according to the number of brain lesions: is stereotactic radiosurgery effective for multiple brain metastases. J Neurosurg. 2010; 113:Suppl. 73–78.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to use Leksell GammaPlan
- Gamma knife radiosurgery for malignant tumors
- Long Term Survival in Patient with Hepatocellular Carcinoma after Surgical Resection of Brain Metastasis: A Case Report
- Gamma Knife Radiosurgery for Single & Multiple brain Metastasis
- Clinical Application of 7.0 T Magnetic Resonance Images in Gamma Knife Radiosurgery for a Patient with Brain Metastases