Infect Chemother.
2012 Aug;44(4):269-274. 10.3947/ic.2012.44.4.269.
Is it Acceptable to Select Antibiotics for the Treatment of Community-acquired Acute Cystitis Based on the Antibiotics Susceptibility Results for Uropathogens from Community-acquired Acute Pyelonephritis in Korea?
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University, College of Medicine, Seoul, Korea. paihj@hanyang.ac.kr
- 2Department of Internal Medicine, Catholic University, College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Gacheon University, College of Medicine, Gacheon, Korea.
- 4Department of Internal Medicine, Ajou University, College of Medicine, Suwon, Korea.
- 5Department of Internal Medicine, Jeju University, College of Medicine, Jeju, Korea.
- 6Department of Internal Medicine, Sungkyunkwan University, College of Medicine, Seoul, Korea.
- 7Department of Internal Medicine, Hallym University, College of Medicine, Seoul, Korea.
- 8Department of Infectious disease, Patima Hospital, Daegu, Korea.
- 9Department of Internal Medicine, Donga University, College of Medicine, Daegu, Korea.
- 10Department of Internal Medicine, Korea University, College of Medicine, Seoul, Korea.
- 11Department of Internal Medicine, Gyemyeong University, College of Medicine, Daegu, Korea.
- 12Department of Internal Medicine, Inha University, College of Medicine, Incheon, Korea.
- KMID: 2045546
- DOI: http://doi.org/10.3947/ic.2012.44.4.269
Abstract
- BACKGROUND
Uncomplicated acute cystitis (CA-UAC) is one of the most common infections treated with antibiotics in the community. However, few data on etiology of CA-UAC and its susceptibility to antibiotics are available, primarily because, in Korea, insurance does not allow reimbursement for microbiological evaluation of CA-UAC. However, microbiologic data on community-acquired uncomplicated acute pyelonephritis (CA-UAPN) are available. The objective of the study was to evaluate the question of whether microbiologic data on CA-UAPN can be used for treatment of CA-UAC; therefore, etiology and antimicrobial susceptibility were compared between pathogens of CA-UAC and those of CA-UAPN.
MATERIALS AND METHODS
During 2008, 538 CA-UACs and 1,265 CA-UAPNs were recruited retrospectively from 14 hospitals (UTI research group). Microbiologic data on etiology and susceptibility to antibiotics were collected retrospectively.
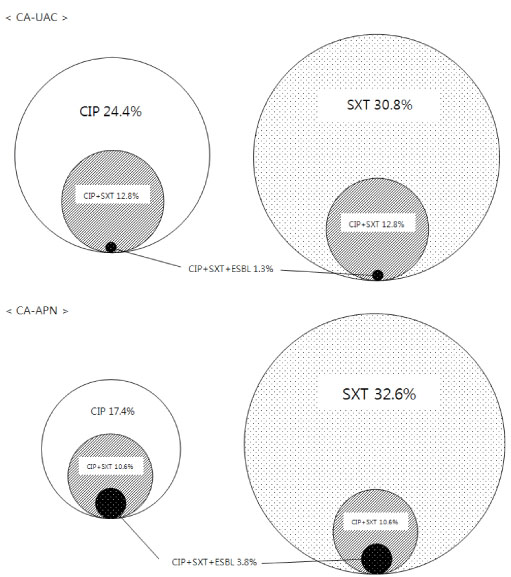
RESULTS
Urine culture was positive in 131 CA-UACs (131/469, 27.9%) and 719 CA-UAPNs (719/1249, 57.6%). Escherichia coli was the most common pathogen in both groups [83.2% (109/131) in CA-UAC vs. 91.9% (661/719) in CA-UAPN]. Susceptibility to common UTI regimens, such as ciprofloxacin, extended-spectrum cephalosporins, and trimethoprim/sulfamethoxazole did not differ between urinary pathogens of CA-UACs and CA-UAPNs, however, a significant difference was observed in rates of resistance to ampicillin/sulbactam (16.5% vs. 42.9%, P<0.001, respectively).
CONCLUSIONS
Rates of resistance of E. coli from CA-UAC and CA-UAPN to most antibiotics did not differ. For proper treatment, further microbiological evaluation for CA-UAC is mandatory.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
The Choice of Empirical Treatment of Uncomplicated Cystitis: No Longer Free Ride
Tae Hyong Kim
Infect Chemother. 2012;44(4):323-327. doi: 10.3947/ic.2012.44.4.323.The Choice of Empirical Treatment of Uncomplicated Cystitis: No Longer Free Ride
Tae Hyong Kim
Infect Chemother. 2012;44(4):323-327. doi: 10.3947/ic.2012.44.4.323.Clinical Practice Guidelines for the Antibiotic Treatment of Community-Acquired Urinary Tract Infections
Cheol-In Kang, Jieun Kim, Dae Won Park, Baek-Nam Kim, U-Syn Ha, Seung-Ju Lee, Jeong Kyun Yeo, Seung Ki Min, Heeyoung Lee, Seong-Heon Wie
Infect Chemother. 2018;50(1):67-100. doi: 10.3947/ic.2018.50.1.67.
Reference
-
1. Nicolle LE. Urinary tract infection: traditional pharmacologic therapies. Am J Med. 2002. 113:Suppl 1A. 35S–44S.
Article2. Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE. Infectious Diseases Society of America. European Society for Microbiology and Infectious Diseases. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011. 52:e103–e120.
Article3. The Korean Society of Infectious Diseases. The Korean Society for Chemotherapy. Korean Association of Urogenital Tract Infection and Inflammation. The Korean Society of Clinical Microbiology. Clinical guideline for the diagnosis and treatment of urinary tract infections: asymptomatic bacteriuria, uncomplicated & complicated urinary tract infections, bacterial prostatitis. Infect Chemother. 2011. 43:1–25.4. Hooton TM, Stamm WE. Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am. 1997. 11:551–581.
Article5. McNulty CA, Richards J, Livermore DM, Little P, Charlett A, Freeman E, Harvey I, Thomas M. Clinical relevance of laboratory-reported antibiotic resistance in acute uncomplicated urinary tract infection in primary care. J Antimicrob Chemother. 2006. 58:1000–1008.
Article6. Lee SS, Kim Y, Chung DR. Impact of discordant empirical therapy on outcome of community-acquired bacteremic acute pyelonephritis. J Infect. 2011. 62:159–164.
Article7. Hwang BY, Lee JG, Park DW, Lee YJ, Kim SB, Eom JS, Sohn JW, Cheong HJ, Kim WJ, Kim MJ, Park SC. Antimicrobial susceptibility of causative microorganisms in adults with acute pyelonephritis at one university-affiliated hospital in southwestern Seoul. Infect Chemother. 2003. 35:277–282.8. Wie SH, Chang UI, Kim HW, Kim YS, Kim SY, Hur J, Kim SI, Kim YR, Kang MW. Clinical features and antimicrobial resistance among clinical isolates of women with community-acquired acute pyelonephritis in 2001-2006. Infect Chemother. 2007. 39:9–16.9. Wie SH, Choi SM, Lee DG, Kim SY, Kim SI, Yoo JH, Shin WS, Kang MW. Antibiotic sensitivity of the causative organisms and use of antibiotics in women with community-acquired acute pyelonephritis. Korean J Infect Dis. 2002. 34:353–359.10. Karlowsky JA, Hoban DJ, Decorby MR, Laing NM, Zhanel GG. Fluoroquinolone-resistant urinary isolates of Escherichia coli from outpatients are frequently multidrug resistant: results from the North American Urinary Tract Infection Collaborative Alliance-Quinolone Resistance study. Antimicrob Agents Chemother. 2006. 50:2251–2254.
Article11. Shin J, Kim J, Wie SH, Cho YK, Lim SK, Shin SY, Yeom JS, Lee JS, Kweon KT, Lee H, Cheong HJ, Park SH, Park DW, Ryu SY, Chung MH, Yoo S, Pai H. Fluoroquinolone resistance in uncomplicated acute pyelonephritis: epidemiology and clinical impact. Microb Drug Resist. 2012. 18:169–175.
Article12. Kim ME, Ha US, Cho YH. Prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in female outpatients in South Korea: a multicentre study in 2006. Int J Antimicrob Agents. 2008. 31:Suppl 1. S15–S18.
Article13. Johnson DE, Lockatell CV, Russell RG, Hebel JR, Island MD, Stapleton A, Stamm WE, Warren JW. Comparison of Escherichia coli strains recovered from human cystitis and pyelonephritis infections in transurethrally challenged mice. Infect Immun. 1998. 66:3059–3065.
Article14. Johnson JR, Owens K, Gajewski A, Kuskowski MA. Bacterial characteristics in relation to clinical source of Escherichia coli isolates from women with acute cystitis or pyelonephritis and uninfected women. J Clin Microbiol. 2005. 43:6064–6072.
Article15. Johnson JR, Kuskowski MA, Gajewski A, Soto S, Horcajada JP, Jimenez de Anta MT, Vila J. Extended virulence genotypes and phylogenetic background of Escherichia coli isolates from patients with cystitis, pyelonephritis, or prostatitis. J Infect Dis. 2005. 191:46–50.
Article16. Kim KY, Kim CS, Lim DH. The ciprofloxacin resistance pattern of Escherichia coli isolated from female patients with community-acquired urinary tract infection in the Jeonnam and Gwangju region for the recent 2-years. Korean J Urol. 2008. 49:540–548.
Article17. Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev. 2005. 18:657–686.18. Lee SE, Choi H, Kim YK. A clinical study of oral fosfomycin (fosmycin) in the treatment of lower urinary tract infection. Korean J Urol. 1984. 25:167–172.19. Ryu KH, Kim MK, Jeong YB. A recent study on the antimicrobial sensitivity of the organisms that cause urinary tract infection. Korean J Urol. 2007. 48:638–645.
Article20. Lee YW, Chang SK. Clinical efficacy of pivmecillinam (Selexid TM) in lower urinary tract infections. Korean J Urol. 1983. 24:413–417.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Community-Acquired Uncomplicated Urinary Tract Infection
- Quinolone Resistance in Community-Acquired Acute Pyelonephritis
- Community Acquired Pneumonia
- Impact of Inappropriate Empirical Antibiotic on Outcomes in Community-acquired Third Generation Cephalosporin Resistant Enterobacterales Bacteremia
- Causative Organisms and Antibiotics Sensitivity in Community Acquired Acute Pyelonephritis