J Korean Soc Magn Reson Med.
2011 Apr;15(1):77-81. 10.13104/jksmrm.2011.15.1.77.
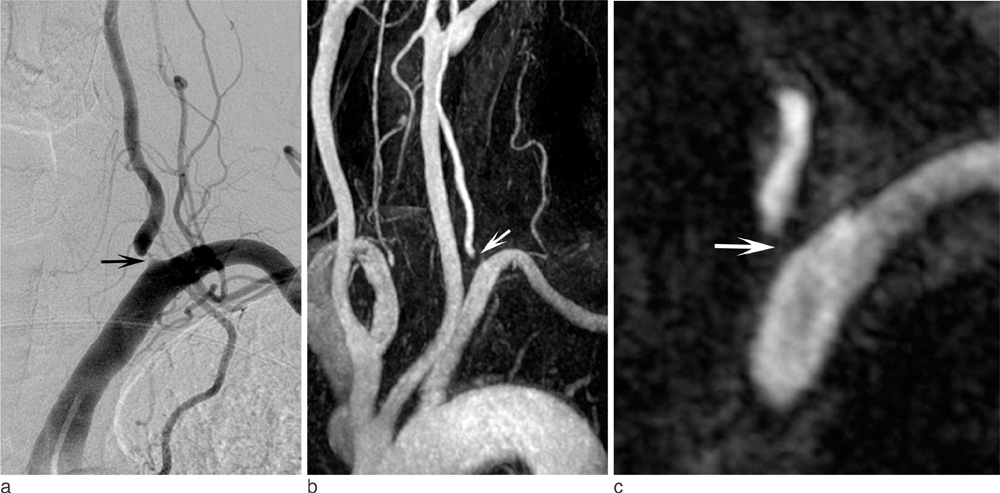
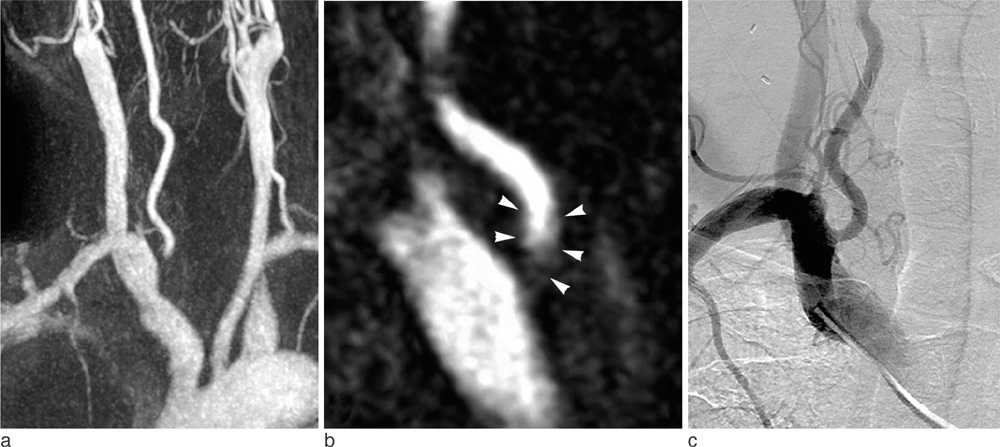
Diagnosis of Vertebral Artery Ostial Stenosis on Contrast-Enhanced MR Angiography: Usefulness of a Thin-Slab MIP Technique
- Affiliations
-
- 1Department of Radiology, Kyung Hee University Hospital-Gangdong, School of Medicine, Kyung Hee University, Seoul, Korea.
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. dhlee@amc.seoul.kr
- 3Department of Radiology, Konkuk University Hospital, Konkuk University School of Medicine, Seoul, Korea.
- 4Department of Radiology, Seoul National University Bundang Hospital, Korea.
- 5Department of Radiology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2041231
- DOI: http://doi.org/10.13104/jksmrm.2011.15.1.77
Abstract
- It is a well-known clinical fact that contrast-enhanced magnetic resonance angiography exaggerates vertebral arterial ostial stenosis and sometimes shows pseudostenosis. Considering the clinical significance of a lesion in the posterior circulation ischemia, the importance of an accurate imaging diagnosis of ostial stenosis should not be underestimated. We were able to differentiate pseudostenosis of the ostium from true stenosis using thin-slab maximum-intensity-projection(MIP) images which are thought to be helpful for minimizing standard full thickness MIP images.
Figure
Reference
-
1. Kollias SS, Binkert CA, Ruesch S, Valavanis A. Contrast-enhanced MR angiography of the supra-aortic vessels in 24 seconds: a feasibility study. Neuroradiology. 1999. 41:391–400.2. Phan T, Huston J 3rd, Bernstein MA, Riederer SJ, Brown RD Jr. Contrast-enhanced magnetic resonance angiography of the cervical vessels: experience with 422 patients. Stroke. 2001. 32:2282–2286.3. Randoux B, Marro B, Koskas F, Chiras J, Dormont D, Marsault C. Proximal great vessels of aortic arch: comparison of three-dimensional gadolinium-enhanced MR angiography and digital subtraction angiography. Radiology. 2003. 229:697–702.4. Remonda L, Senn P, Barth A, Arnold M, Lovblad KO, Schroth G. Contrast-enhanced 3D MR angiography of the carotid artery: comparison with conventional digital subtraction angiography. AJNR Am J Neuroradiol. 2002. 23:213–219.5. Leclerc X, Martinat P, Godefroy O, et al. Contrast-enhanced three-dimensional fast imaging with steady-state precession (FISP) MR angiography of supraaortic vessels: preliminary results. AJNR Am J Neuroradiol. 1998. 19:1405–1413.6. Slosman F, Stolpen AH, Lexa FJ, et al. Extracranial atherosclerotic carotid artery disease: evaluation of non-breath-hold three-dimensional gadolinium-enhanced MR angiography. AJR Am J Roentgenol. 1998. 170:489–495.7. Cosottini M, Calabrese R, Puglioli M, et al. Contrast-enhanced three-dimensional MR angiography of neck vessels: does dephasing effect alter diagnostic accuracy? Eur Radiol. 2003. 13:571–581.8. Chung TS, Lee YJ, Kang WS, et al. Clinical and experimental investigation of pseudoaneurysm in the anterior communicating artery area on 3-dimensional time-of-flight cerebral magnetic resonance angiography. J Comput Assist Tomogr. 2004. 28:414–421.9. Evans AJ, Richardson DB, Tien R, et al. Poststenotic signal loss in MR angiography: effects of echo time, flow compensation, and fractional echo. AJNR Am J Neuroradiol. 1993. 14:721–729.10. Neri E, Cosottini M, Caramella D. MR angiography of the body: technique and applications. 2010. Heidelberg: Springer;36–39.11. Caplan LR, Wityk RJ, Glass TA, et al. New England Medical Center Posterior Circulation registry. Ann Neurol. 2004. 56:389–398.12. Hankey GJ, Warlow CP, Sellar RJ. Cerebral angiographic risk in mild cerebrovascular disease. Stroke. 1990. 21:209–222.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Coronary Ostial Stenosis Confirmed by Transesophageal Echocardiogram: A Case Report
- Usefulness of MR Angiography in Patients with Ischemic Stroke
- Comparison of Transaxial Source Images and 3-Plane, Thin-Slab Maximal Intensity Projection Images for the Diagnosis of Coronary Artery Stenosis with Using ECG-Gated Cardiac CT
- Dynamic Contrast-Enhanced T2*-Weighted Imaging in Acute Cerebral Infarction: Usefulness in Assessment of Cerebral Hemodynamics
- Pseudostenosis at the Origin of the Vertebral Artery on Contrast-enhanced MRA: Correlation with Aortic Motion on Dynamic 3D Time-Resolved Contrast-Enhanced MRA