J Korean Soc Spine Surg.
2006 Mar;13(1):48-53. 10.4184/jkss.2006.13.1.48.
The Evaluation of Bony Union after Posterior Occipitocervical Fusion
- Affiliations
-
- 1Spine Center, Department of Orthopaedic Surgery, Sun General Hospital, Daejeon, Korea. hc5771@chollian.net
- 2Department of Orthopaedic Surgery, The Catholic University of Korea, College of Medicine, Seoul, Korea.
- KMID: 2040780
- DOI: http://doi.org/10.4184/jkss.2006.13.1.48
Abstract
-
STUDY DESIGN: The results of posterior occipitocervical fusions were analyzed retrospectively based on the results of post-operative radiographs.
OBJECTIVES
To investigate subjective methods for the evaluation of occipitocervical stabilization by posterior fusion. SUMMARY OF LITERATURE REVIEW: Few studies have been performed that describe the methods utilized for the evaluation of the union of the instrumented segments.
MATERIALS AND METHODS
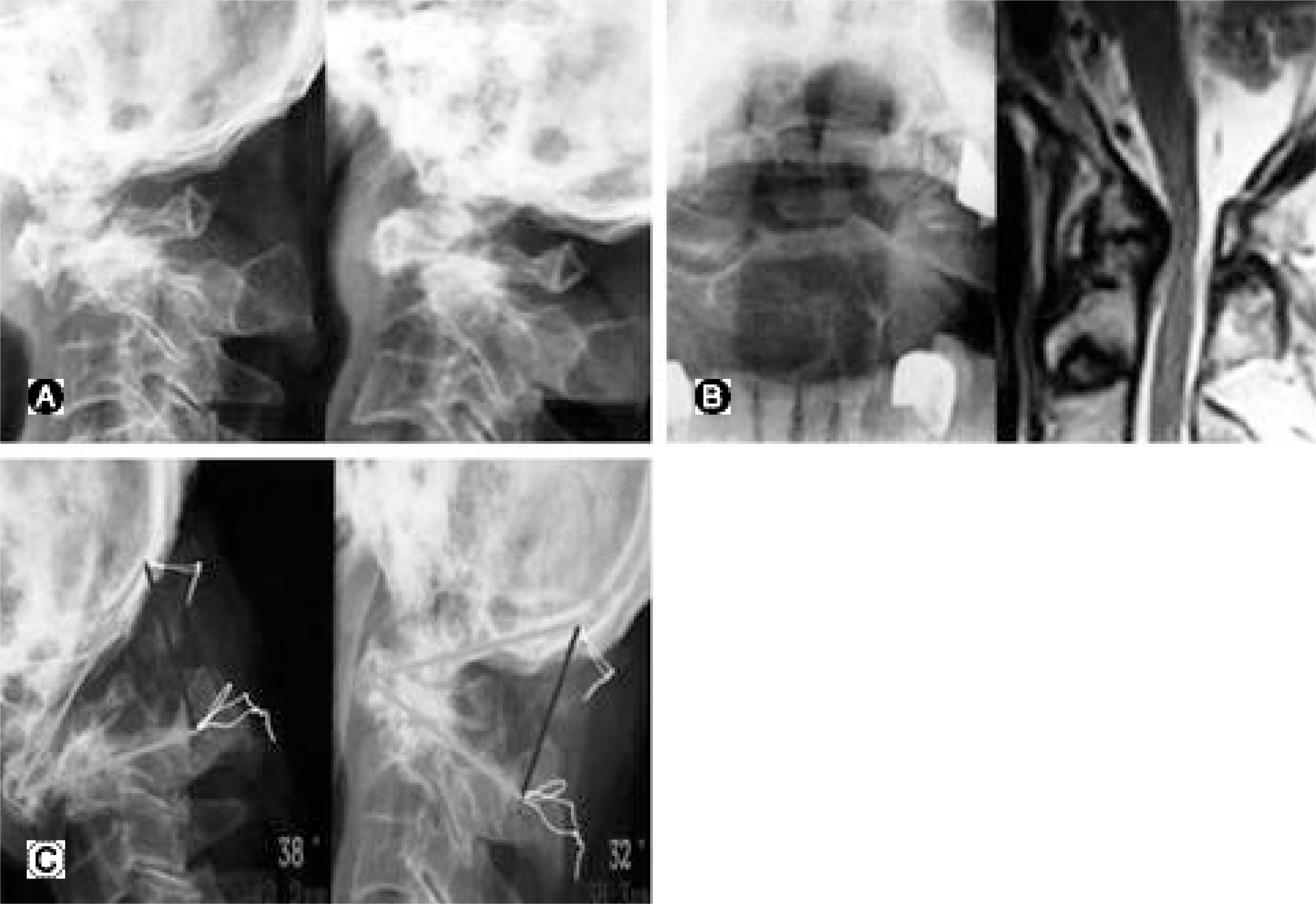
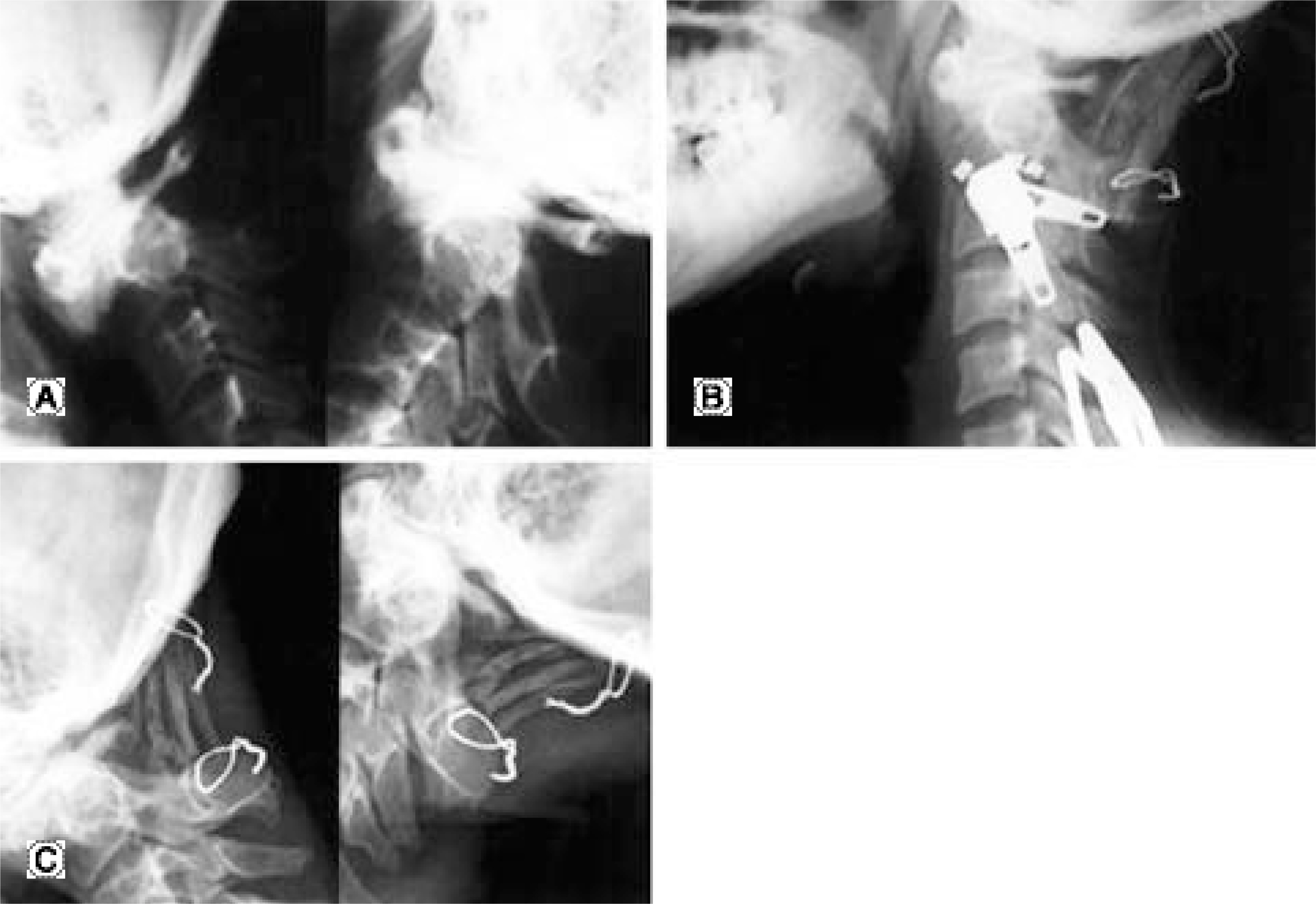
Occipitocervical fusions were performed in 16 patients from 1995 to 2004. The patients underwent occipitocervical fusions with autogenous iliac bone grafting and wire fixation (5), loop and sublaminar wire fixation (3), C-D occipitocervical rod (2), and contoured reconstruction plate (6). The stability and failure of the instrumentation in the fusion sites were evaluated with flexion/extension lateral radiographs. The stability was evaluated by a change in the degrees and distances between the occiput and cervical vertebrae.
RESULTS
Two of five patients who had undergone wire fixation with autogenous bone grafting were considered to have a nonunion because of persistent segmental instability: greater than 2 degrees and 2 mm three months postoperatively. In the other patients, we were unable to determine the presence of a solid fusion mass at the fusion site, because of overlapping of the instrumentation devices and graft bones. However, since there was no definite motion that indicated segmental instability and instrumentation breakage or loosening on flexion and extension radiographs, we considered these as stable fixations.
CONCLUSION
It was difficult to evaluate whether or not the grafts were incorporated into the recipient sites, due to the complexity of the occipitocervical junction and the overlapping of the instrumentation. After removal of the external immobilization 3 months postoperatively, although flexion/extension radiographs taken 6 months postoperatively, demonstrated no motion at the fusion site, the occipitocervical fusions were judged to be stabilized rather than fused.
MeSH Terms
Figure
Reference
-
1). Bohlman HH. Occipitocervical fusion. J Bone Joint Surg Am. 1987; 69:833–836.2). Elia M, Mazzara JT, Fielding JW. Onlay technique for occipitocervical fusion. Clin Orthop. 1992; 280:170–174.
Article3). Wetheim SB, Bohlman HH. Occipitocervical fusions: indications, techniques, and long-term results in 13 patients. J Bone Joint Surg Am. 1987; 69:833–836.4). Itoh T, Tsuji H, Katoh Y, Yonezaua T, Kitagawa H. Occipitocervical fusion reinforced by Luque's segmental spinal instrumentation for rheumatoid diseases. Spine. 1988; 13:1234–1238.
Article5). Mackenzie AI, Uttley D, Marsh HT, Bell BA. Cranio -cervical stabilization using Luque/Hartshill rectangles. Neurosurg. 1990; 26:32–36.6). Malcolm AI, Ransford JR, Crockard HA. Treatment of non-rheumatoid occipitocervical instability. Internal fixation with the Hartshill-Ransford loop. J Bone Joint Surg Br. 1994; 76:357–366.
Article7). Sakou T, Matsunaga S. Occipitoatlantoaxial fusion uti -lizing a rectangular rod. Clin Orthop. 1989; 239:136–144.8). Grob D, Dvorak J, Panjabi MM, Anthnes JA. The role of plate and screw fixation in occipitocervical fusion in rheumatoid arthritis. Spine. 1994; 19:2545–2551.
Article9). Heidecke V, Rainov R, Burkert W. Occipi tocervical fusion with the cervical Cotrel-Dubousset rod system. Acta Neurochir(Wien). 1998; 140:969–976.10). McAfee PC, Cassidy JR, Davis RF, et al. Fusion of the occiput to the upper cervical spine. Spine. 1991; 16:S490–S494.
Article11). Paquis P, Breuil V, Lonjon M, Euller-Ziegler L, Grelli-er P. Occipitocervical fixation using hooks and screws for upper cervical instability. Neurosurg. 1999; 44:324–330.
Article12). Sasso RC, Jeanneret B, Fischer K, Magerl F. Occipitocervical fusion with posterior plate and screw instrumentation. Spine. 1994; 19:2364–2468.13). Smith MD, Anderson P, Grady MS. Occipito cer vical arthrodesis using contoured plate fixation. Spine. 1993; 18:1984–1990.14). Clark CR. Occipitocervical fusion for the unstable rheumatoid neck. Orthopedics. 1989; 12:469–473.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dysphagia after Occipitocervical Posterior Fusion and Significance of Occipitoaxial Angle: case report
- Dyspnea and Dysphagia after Posterior Atlantoaxial Instrumented Fusion
- Double Plate Occipitocervical Fusion After Failed Posterior Fusion C 1-2 With Wiring
- Occipito-Cervical Fusion Reinforced by C-D Occipitocervical Loop
- Autogenic Rib Graft for Atlantoaxial and Occipitocervical Fixation in Pediatric Patients