J Korean Neurosurg Soc.
2012 Nov;52(5):498-500. 10.3340/jkns.2012.52.5.498.
Infection of Cranioplasty Seen Twenty Years Later
- Affiliations
-
- 1Department of Neurosurgery, Haydarpasa Numune Education and Research Hospital, Istanbul, Turkey. mehmetsabrigurbuz@gmail.com
- KMID: 2018261
- DOI: http://doi.org/10.3340/jkns.2012.52.5.498
Abstract
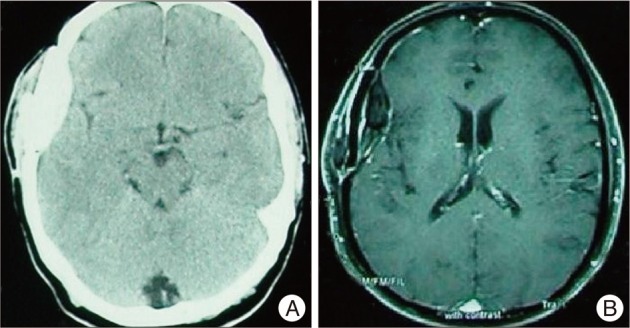
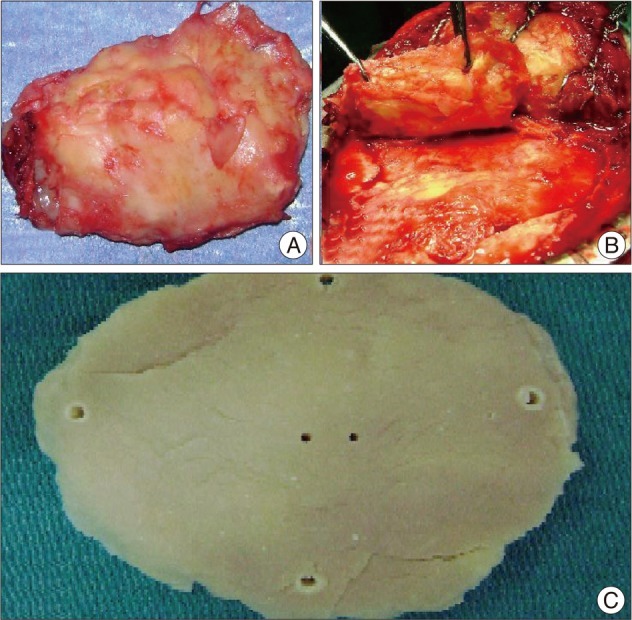
- Cranioplasty is performed using autograft and allograft materials on patients to whom craniectomy was applied previously due to the facts that, this region is open to trauma and the scalp makes irritation and pressure onto the brain paranchyma causing brain atrophy and convulsions. Dramatical improvement of neurological deficits, control of convulsions and partial prevention of cerebral atrophy are achieved after these operations. One of the most important complications of cranioplasty is late infection. Here, we report a 43-year-old male patient admitted with the history of purulant discharge from the right temporal incission site for one year to whom cranioplasty had been performed with allograft material 20 days after craniectomy which had been performed in 1989. Allograft cranioplasty material was removed and cranioplasty was performed using new allograft material with the diagnosis of late cranioplasty infection.
Figure
Reference
-
1. Benzel EC, Thammavaram K, Kesterson L. The diagnosis of infections associated with acrylic cranioplasties. Neuroradiology. 1990; 32:151–153. PMID: 2398941.
Article2. Brett-Major DM, Baraniak SM, Gilhooly JE, Christensen RL, Grant GT, Armonda RA, et al. Foreign-body reaction mimicking postneurosurgical infection after cranioplasty. Mil Med. 2008; 173:697–699. PMID: 18700607.
Article3. Cheng YK, Weng HH, Yang JT, Lee MH, Wang TC, Chang CN. Factors affecting graft infection after cranioplasty. J Clin Neurosci. 2008; 15:1115–1119. PMID: 18656363.
Article4. Edwards MSB, Ousterhout DK. Autogeneic skull bone grafts to reconstruct large or compleks skull defects in children and adolescents. Neurosurgery. 1987; 20:273–280. PMID: 3561736.
Article5. Gladstone HB, McDermott MW, Cooke DD. Implants for cranioplasty. Otolaryngol Clin North Am. 1995; 28:381–400. PMID: 7596618.
Article6. Hammon WM, Kempe LG. Methyl methacrylate cranioplasty. 13 years experience with 417 patients. Acta Neurochir (Wien). 1971; 25:69–77. PMID: 5135756.7. Matsuno A, Tanaka H, Iwamuro H, Takanashi S, Miyawaki S, Nakashima M, et al. Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir (Wien). 2006; 148:535–540. discussion 540. PMID: 16467959.
Article8. Morioka T, Fujiwara S, Akimoto T, Nishio S, Fukui M. Intracranial epidural abscess : late complication of allograft cranioplasty. Fukuoka Igaku Zasshi. 1996; 87:57–59. PMID: 8851369.9. Rish BL, Dillon JD, Meirowsky AM, Caveness WF, Mohr JP, Kistler JP, et al. Cranioplasty : a review of 1030 cases of penetrating head injury. Neurosurgery. 1979; 4:381–385. PMID: 111153.10. Sakai H, Kanki T, Fuse T, Nakamura N. [Head injuries in patients with pre-existing skull defects]. No Shinkei Geka. 1983; 11:1093–1096. PMID: 6646341.11. Schuss P, Vatter H, Marquardt G, Imöhl L, Ulrich CT, Seifert V, et al. Cranioplasty after decompressive craniectomy : the effect of timing on postoperative complications. J Neurotrauma. 2012; 29:1090–1095. PMID: 22201297.
Article12. Şekerci Z, Çolpan E. Kranioplastiler. Temel Nöroşirürji, cilt 1. 2005. birinci baskı, Ankara: Türk Nöroşirürji Derneği Yayınları;p. 246–257.13. Thavarajah D, De Lacy P, Hussien A, Sugar A. The minimum time for cranioplasty insertion from craniectomy is six months to reduce risk of infection--a case series of 82 patients. Br J Neurosurg. 2012; 26:78–80. PMID: 21973063.
Article14. Tokoro K, Chiba Y, Tsubone K. Late infection after cranioplasty--review of 14 cases. Neurol Med Chir (Tokyo). 1989; 29:196–201. PMID: 2477724.15. Yamaura A, Sato M, Meguro K, Nakamura T, Uemura K. [Cranioplasty following decompressive craniectomy--analysis of 300 cases (author's transl)]. No Shinkei Geka. 1977; 5:345–353. PMID: 558536.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Infection Following Cranioplasty: Review of 4 Cases
- Which One Is Better to Reduce the Infection Rate, Early or Late Cranioplasty?
- Review of Cranioplasty after Decompressive Craniectomy
- Long-Term Incidence and Predicting Factors of Cranioplasty Infection after Decompressive Craniectomy
- A Clinical Study on Cranioplasty