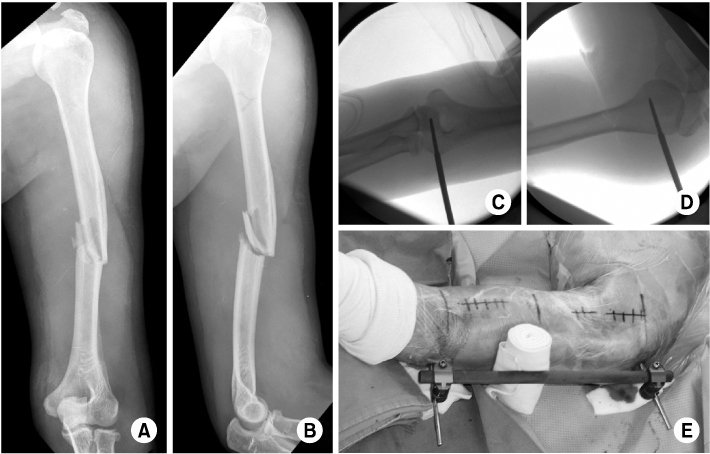
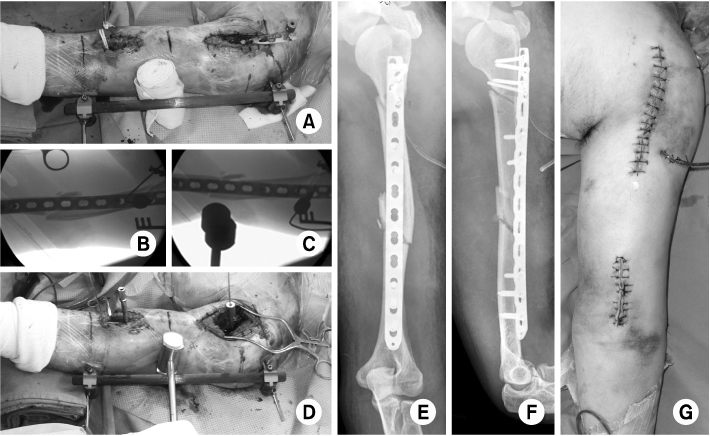
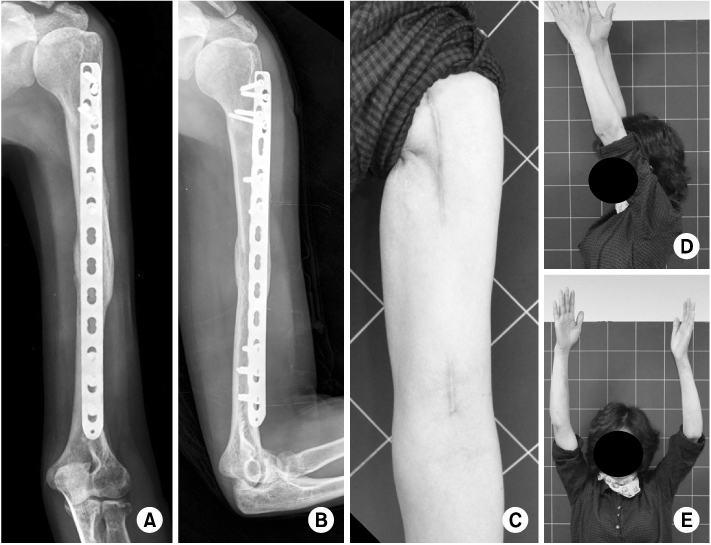
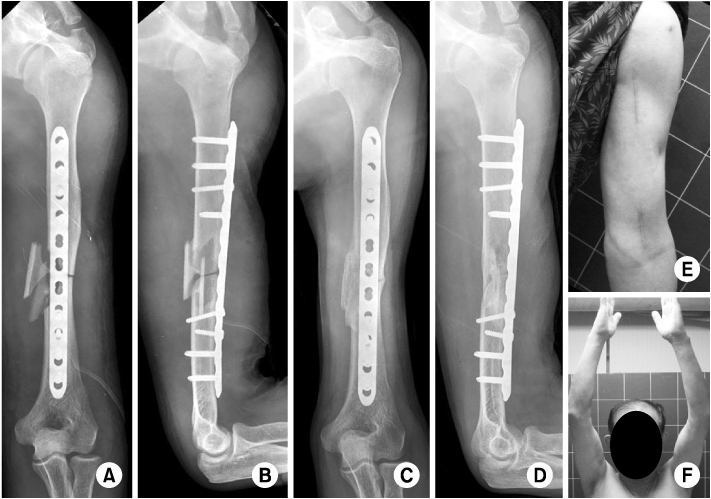
Operative Treatment of Humerus Shaft Fracture: Conventional Open Plating or Minimally Invasive Plate Osteosynthesis
- Affiliations
-
- 1Department of Orthopedic Surgery, Kyungpook National University Hospital, Daegu, Korea. cwoh@knu.ac.kr
- KMID: 2015461
- DOI: http://doi.org/10.12671/jkfs.2012.25.2.155
Abstract
- No abstract available.
MeSH Terms
Figure
Cited by 3 articles
-
Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
Hyoung Keun Oh, Suk Kyu Choo, Jung Il Lee, Dong Hyun Seo
J Korean Fract Soc. 2012;25(4):305-309. doi: 10.12671/jkfs.2012.25.4.305.Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
Hyoung Keun Oh, Suk Kyu Choo, Jung Il Lee, Dong Hyun Seo
J Korean Fract Soc. 2012;25(4):305-309. doi: 10.12671/jkfs.2012.25.4.305.Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
Youn-Soo Hwang, Kwang-Yeol Kim, Hyung-Chun Kim, Su-Han Ahn, Dong-Eun Lee
J Korean Fract Soc. 2013;26(1):14-20. doi: 10.12671/jkfs.2013.26.1.14.
Reference
-
1. An Z, Zeng B, He X, Chen Q, Hu S. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. Int Orthop. 2010. 34:131–135.2. Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005. 36:530–538.
Article3. Apivatthakakul T, Patiyasikan S, Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: a cadaveric study. Injury. 2010. 41:169–172.
Article4. Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fractures--a meta-analysis. Acta Orthop. 2006. 77:279–284.5. Carlan D, Pratt J, Patterson JM, Weiland AJ, Boyer MI, Gelberman RH. The radial nerve in the brachium: an anatomic study in human cadavers. J Hand Surg Am. 2007. 32:1177–1182.6. Changulani M, Jain UK, Keswani T. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop. 2007. 31:391–395.
Article7. Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000. 14:162–166.
Article8. Chen AL, Joseph TN, Wolinksy PR, et al. Fixation stability of comminuted humeral shaft fractures: locked intramedullary nailing versus plate fixation. J Trauma. 2002. 53:733–737.
Article9. Chiu FY, Chen CM, Lin CF, Lo WH, Huang YL, Chen TH. Closed humeral shaft fractures: a prospective evaluation of surgical treatment. J Trauma. 1997. 43:947–951.
Article10. Concha JM, Sandoval A, Streubel PN. Minimally invasive plate osteosynthesis for humeral shaft fractures: are results reproducible? Int Orthop. 2010. 34:1297–1305.
Article11. Dabezies EJ, Banta CJ 2nd, Murphy CP, d'Ambrosia RD. Plate fixation of the humeral shaft for acute fractures, with and without radial nerve injuries. J Orthop Trauma. 1992. 6:10–13.
Article12. Farragos AF, Schemitsch EH, McKee MD. Complications of intramedullary nailing for fractures of the humeral shaft: a review. J Orthop Trauma. 1999. 13:258–267.
Article13. Herscovici D Jr, Anglen JO, Archdeacon MT, Cannada LK, Scaduto JM. Avoiding complications in the treatment of pronation-external rotation ankle fractures, syndesmotic injuries, and talar neck fractures. Instr Course Lect. 2009. 58:37–45.
Article14. Ji F, Tong D, Tang H, et al. Minimally invasive percutaneous plate osteosynthesis (MIPPO) technique applied in the treatment of humeral shaft distal fractures through a lateral approach. Int Orthop. 2009. 33:543–547.
Article15. Jiang R, Luo CF, Zeng BF, Mei GH. Minimally invasive plating for complex humeral shaft fractures. Arch Orthop Trauma Surg. 2007. 127:531–535.
Article16. Lee HJ, Oh CW, Kim DH, Park KH. Minimally invasive anterior plating of humeral shaft fractures. J Korean Fract Soc. 2011. 24:341–346.17. Lin J, Shen PW, Hou SM. Complications of locked nailing in humeral shaft fractures. J Trauma. 2003. 54:943–949.18. Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004. 35:587–595.
Article19. McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br. 2000. 82:336–339.
Article20. Oh CW, Byun YS, Oh JK, et al. Plating of humeral shaft fractures: Comparison of standard conventional plating versus minimally invasive plating. Orthop Traumatol Surg Res. 2012. 98:54–60.
Article21. Volgas DA, Stannard JP, Alonso JE, et al. Nonunions of the humerus. Clin Orthop Relat Res. 2004. (419):46–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Anterior Plating of Humeral Shaft Fractures
- Clinical Outcomes of Locking Compression Plate Fixation through Minimally Invasive Percutaneous Plate Osteosynthesis in the Treatment of Distal Tibia Fracture
- Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
- Minimal Invasive Plate Osteosynthesis versus Conventional Open Plating in Simple Humeral Shaft Fracture (AO Type A, B1, B2)
- Minimally Invasive Percutaneous Plate Osteosynthesis for Distal Tibial Shaft Fracture