J Korean Soc Spine Surg.
2003 Jun;10(2):137-145. 10.4184/jkss.2003.10.2.137.
Mono-segment Pedicle-screw Instrumentation and Fusion following Vertebroplasty for Lumbar and Thoracolumbar Fractures
- Affiliations
-
- 1Department of Orthopaedic Surgery, Sung-Ae General Hospital, Seoul, Korea. choknm@hanmir.com
- 2Department of Orthopaedic Surgery, Pundang Cha Hospital.
- 3Pochun Jungmoon College of Medicine, Sungnam, Korea.
- KMID: 2003211
- DOI: http://doi.org/10.4184/jkss.2003.10.2.137
Abstract
- STUDY DESIGN: Nineteen of 20 cases that underwent a mono-segment pedicle-screw instrumentation and fusion, following vertebroplasty for lumbar and thoracolumbar fractures, were reviewed retrospectively.
OBJECTIVES
To assess the effectiveness of a mono-segment pedicle-screw instrumentation and fusion, following an anterior column reconstruction, using bone cement for a fractured lumbar and thoracolumbar spine. SUMMARY OF LITERATURE REVIEW: With lumbar and thoracolumbar fractures, the untreated anterior instability and pre-stressing of the screws, following reduction, resulted in a high failure rate of the hardware, and posterior screw fixation alone may be not adequate.
MATERIALS AND METHODS
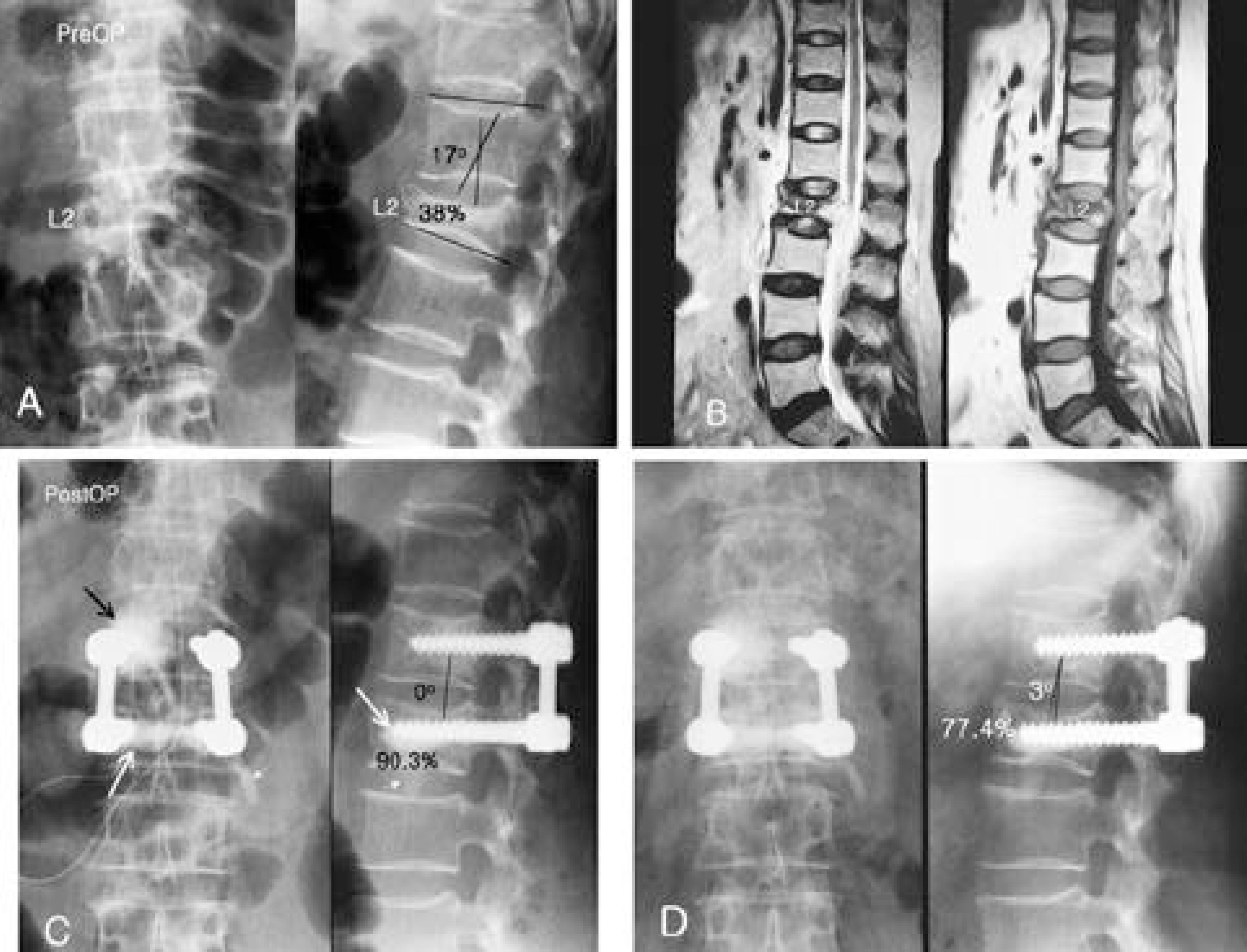
We reviewed 19 of 20 cases that underwent a mono-segment pedicle-screw instrumentation and fusion, following vertebroplasty for lumbar and thoracolumbar fractures, between Feb. 2000 and Mar. 2002, with an average follow-up of 1.6 years. The mean age of the patients was 39.2 years, and the male female ratio as 10:9. The criteria for inclusion to the study (McAfee classification) were flexion-distraction injury, burst fracture, translational injury and burst conversion after an osteoporotic compression fracture, in 9, 7, 2 and 2 cases, respectively. We assessed the radiographic results of the local kyphotic angle correction of the fused segment and anterior body height restoration, preoperative, postoperative and at the last follow up, from the lateral views of the spine. The clinical results were evaluated according to Kumano's criteria.
RESULTS
The mean local kyphotic angles of the instrumented segment, preoperatively, postoperatively and at the last follow-up were 16.5, 1.1 and 2.1 degrees, with a mean correction gain of 15.4 degrees(p<0.05) and a gain loss of 1.0 degrees(p>0.05). The mean anterior body heights for each period were 60.4, 89.6 and 85.0%, with a mean restoration gain of 29.2% (p<0.05) and a gain loss of 4.6% (p>0.05). The clinical results were assessed as good in 18 patients (19 cases) and fair in the other one. There were 3 cases of asymptomatic leakage of the bone cement, but no fixation failures during the follow-up.
CONCLUSIONS
A mono-segment pedicle-screw instrumentation and fusion, following the treatment of anterior instability, using vertebroplasty for lumbar and thoracolumbar fractures, can be an effective alternative for preserving the maximal motion segment, without fixation loss through the restoration of the immediate postoperative weight-bearing capability.
MeSH Terms
Figure
Reference
-
1). Brantigan JW., Steffee AD., Lewis ML., Quinn LM., Persenaire JM. Lumbar interbody fusion using the Brantigan I/F Cage for posterior lumbar interbody fusion and the variable pedicle screw placement system. Spine,. 25:1437–1446. 2000.
Article2). Carl AL., Tromanhauser SG., Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine,. 17:317–324. 1992.
Article3). Dekutoski MB., Conlan ES., Salciccioli GG. Spinal mobility and deformity after Harrington rod stabilization and limited arthrodesis of thoracolumbar fractures. J Bone Joint Surg,. 75:168–176. 1993.
Article4). Dickson JH., Harrington PR., Erwin WD. Results of reduction and stabilization of the severely fractured tho -racic and lumbar spine. J Bone Joint Surg,. 59-A:143–153. 1977.5). Ebelke DK., Asher MA., Neff JR., Kraker DP. Sur -vivorship analysis of VSP spine instrumentation in the treatment of thoracolumbar and lumbar burst fractures. Spine. 16:428–432. 1991.6). Grubb SA., Lipscomb HJ. Results of lumbosacral fusion for degenerative disc disease with and without instrumentation-two to five year follow-up. Spine,. 17:349–355. 1992.7). Gurwitz GS., Dawson JM., McNamara MJ., Federspiel CF., Spengler DM. Biomechanical analysis of three surgical approaches for lumbar burst fractures using short-segment instrumentation. Spine,. 18:977–982. 1993.
Article8). Kumano K., Hirabayashi S., Ogawa Y., Aota Y. Pedicle Screws and Bone Mineral Density. Spine,. 19:1157–1161. 1994.
Article9). Mann KA., Mcgowan DP., Fredrickson BE., Falahee M., Yuan HA. A biomechanical investigation of short segment spinal fixation for burst fractures with varying degree posterior disruption. Spine. 15:470–478. 1990.10). McLain RF., Sparling E., Benson DR. Early failure of short-segment pedicle instrumentation for thoracolum -bar fractures. J Bone Joint Surg,. 75:162–7. 1993.11). Mermelstein LE., Mclain RF., Yerby SA. Reinforce -ment of thoracolumbar burst fractures with calcium phos -phate cement. Spine,. 23:664–671. 1998.12). Muller U., Berlemann U., Sledge J., Schwarzenbach O. Treatment of thoracolumbar burst fractures without neurologic deficit by indirct reduction and posterior instrumentation: bisegmental stabilization with monoseg -mental fusion. Eur Spine,. 8:284–289. 1999.13). Parker JW., Lane JR., Karaikovic EE., Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures. Spine,. 25:1157–1169. 2000.
Article14). Verlaan JJ., Helden WH., Oner FC., Verbout AJ., Dhert WJA. Balloon vertebroplasty with calcium phos -phate cement augmentation for direct restoration of trau -matic thoracolumbar vertebral fractures. Spine,. 27:543–548. 2002.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long Segment Pedicle Instrumentation and Anterior Interbody Fusion for Thoraclumbar Burst Fractures
- Decision of Posterior Fixation Level by Load-Sharing Classification in Thoracolumbar and Lumbar Burst Fracture
- Unilateral versus Bilateral Pedide Scrwe Fixation in Lumbar Spinal Fusion
- Short- and Long-segment Pedicle Screw Fixation with Anterior Interbody Fusion with Short Bone Graft in Denis type B Burst Fractures
- Short Segment Pedicle Screw Fixation with Augmented Intra-Operative Vertebroplasty in Unstable Thoraco-Lumbar Fracture: Preliminary Report