J Korean Soc Radiol.
2010 May;62(5):483-490. 10.3348/jksr.2010.62.5.483.
Micro-CT Arthrographic Analysis of Monosodium Iodoacetate-Induced Osteoarthritis in Rat Knees
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
- 2Department of Radiology, Seoul National University Bundang Hospital, Korea. kanghs@radcom.snu.ac.kr
- 3Department of Radiology and Institute of Radiation Medicine, Seoul National University College of Medicine, Korea.
- KMID: 2002958
- DOI: http://doi.org/10.3348/jksr.2010.62.5.483
Abstract
- PURPOSE
To evaluate the arthrographic findings of MIA-induced osteoarthritis in rat knees using the micro-CT arthrography.
MATERIALS AND METHODS
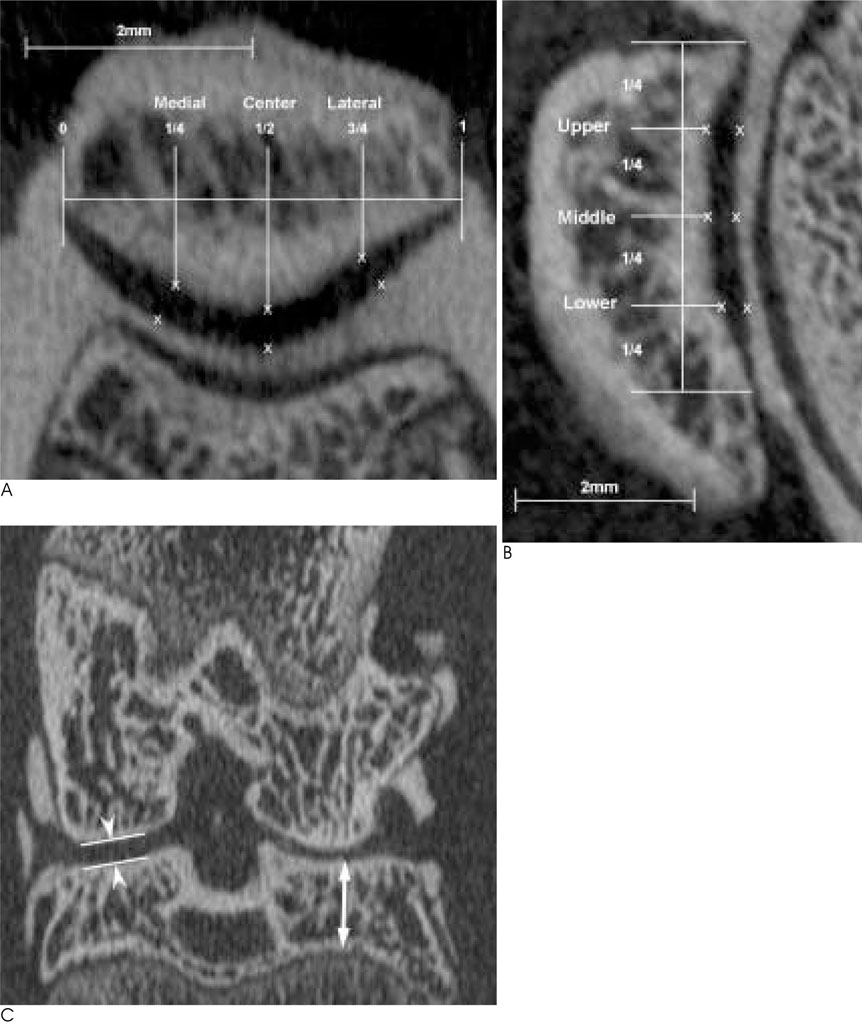
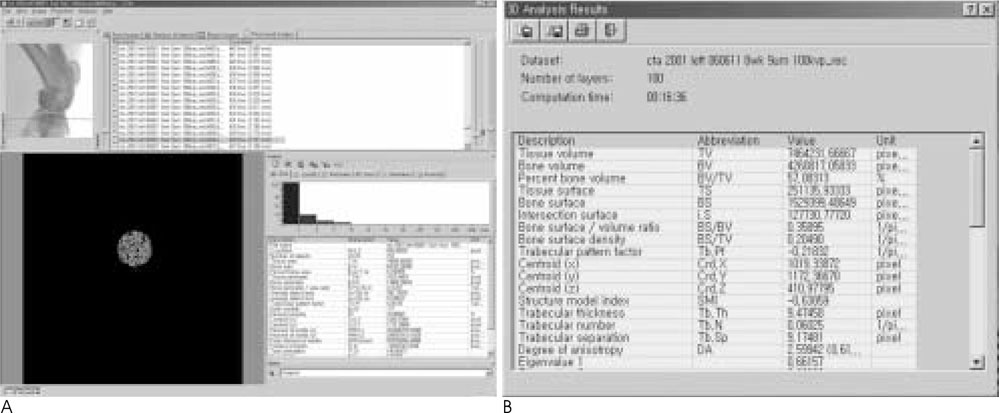
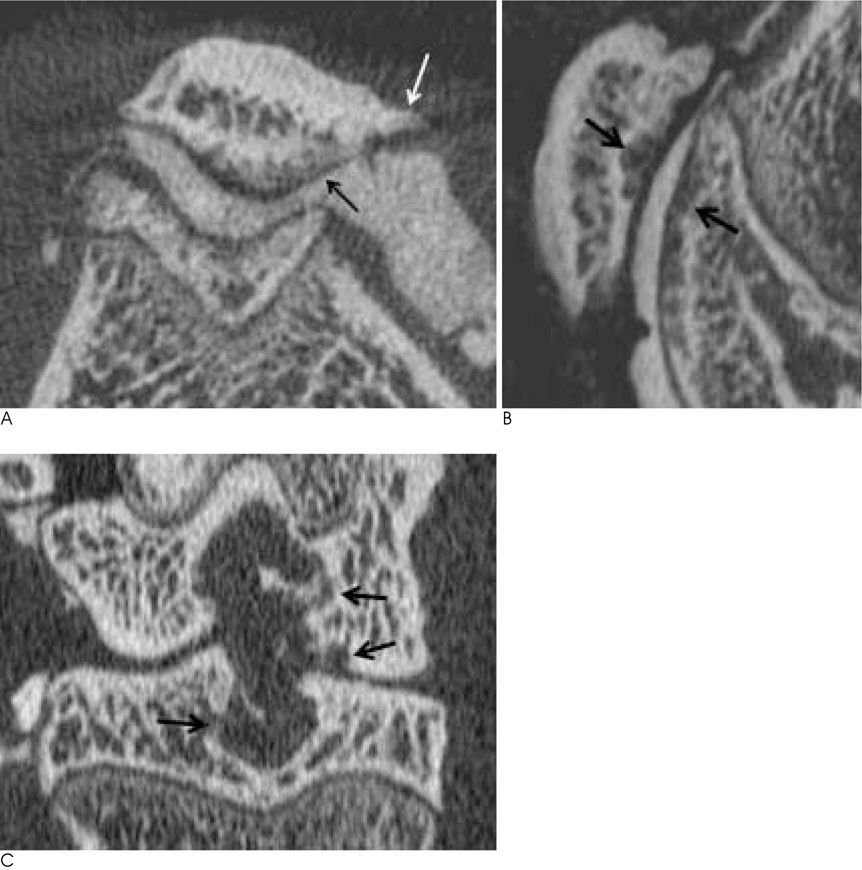
Intra-articular monosodium iodoacetate (MIA) injection-induced arthritis was induced in the right knees of twelve rats; their left knees served as the control group. Eight weeks after MIA injection, micro-CT arthrography was performed on each knee. We measured the thickness of retro-patellar cartilages, the distances of tibio-femoral joint space, subchondral bone plate thickness, tibial epiphyseal height, and transverse patellar diameter. Subchondral trabecular bone indices were measured in the tibial lateral condylar epiphysis. The data were analyzed statistically using a paired t-test.
RESULTS
The retro-patellar articular cartilage showed thinning on the right side that had been induced to develop osteoarthritis. The right knees showed a significant reduction in the distance of the tibio-femoral joint space, prominent patellar osteophytes, and the resorption of subchondral bone. Among the subchondral trabecular bone indices, percent bone volume, and trabecular thickness was reduced on the right side.
CONCLUSION
The articular cartilage thickness of MIA-induced arthritis model could be measured using micro-CT arthrography. It was possible to evaluate the osteoarthritic findings including the change in subchondral bone plate thickness, osteophyte formation, and subchondral bone resorption, as well as quantitatively analyze the trabecular bone indices.
MeSH Terms
Figure
Reference
-
1. Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000; 133:635–646.2. Bendele A, McComb J, Gould T, McAbee T, Sennello G, Chlipala E, et al. Animal models of arthritis: relevance to human disease. Toxicol Pathol. 1999; 27:134–142.3. Guingamp C, Gegout-Pottie P, Philippe L, Terlain B, Netter P, Gillet P. Mono-iodoacetate-induced experimental osteoarthritis: a dose-response study of loss of mobility, morphology, and biochemistry. Arthritis Rheum. 1997; 40:1670–1679.4. Janusz MJ, Hookfin EB, Heitmeyer SA, Woessner JF, Freemont AJ, Hoyland JA, et al. Moderation of iodoacetate-induced experimental osteoarthritis in rats by matrix metalloproteinase inhibitors. Osteoarthritis Cartilage. 2001; 9:751–760.5. Guzman RE, Evans MG, Bove S, Morenko B, Kilgore K. Monoiodoacetate-induced histologic changes in subchondral bone and articular cartilage of rat femorotibial joints: an animal model of osteoarthritis. Toxicol Pathol. 2003; 31:619–624.6. Batiste DL, Kirkley A, Laverty S, Thain LM, Spouge AR, Gati JS, et al. High-resolution MRI and micro-CT in an ex vivo rabbit anterior cruciate ligament transection model of osteoarthritis. Osteoarthritis Cartilage. 2004; 12:614–626.7. Nagele E, Kuhn V, Vogt H, Link TM, Muller R, Lochmuller EM, et al. Technical considerations for microstructural analysis of human trabecular bone from specimens excised from various skeletal sites. Calcif Tissue Int. 2004; 75:15–22.8. Roemer FW, Mohr A, Lynch JA, Meta MD, Guermazi A, Genant HK. Micro-CT arthrography: a pilot study for the ex vivo visualization of the rat knee joint. AJR Am J Roentgenol. 2005; 184:1215–1219.9. Vande Berg BC, Lecouvet FE, Poilvache P, Jamart J, Materne R, Lengele B, et al. Assessment of knee cartilage in cadavers with dual-detector spiral CT arthrography and MR imaging. Radiology. 2002; 222:430–436.10. Bove SE, Calcaterra SL, Brooker RM, Huber CM, Guzman RE, Juneau PL, et al. Weight bearing as a measure of disease progression and efficacy of anti-inflammatory compounds in a model of monosodium iodoacetate-induced osteoarthritis. Osteoarthritis Cartilage. 2003; 11:821–830.11. van der Kraan PM, Vitters EL, van de Putte LB, van den Berg WB. Development of osteoarthritic lesions in mice by “metabolic” and “mechanical” alterations in the knee joints. Am J Pathol. 1989; 135:1001–1014.12. Radin EL, Rose RM. Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop Relat Res. 1986; 34–40.13. Grynpas MD, Alpert B, Katz I, Lieberman I, Pritzker KP. Subchondral bone in osteoarthritis. Calcif Tissue Int. 1991; 49:20–26.14. Li B, Marshall D, Roe M, Aspden RM. The electron microscope appearance of the subchondral bone plate in the human femoral head in osteoarthritis and osteoporosis. J Anat. 1999; 195:101–110.15. Day JS, Ding M, van der Linden JC, Hvid I, Sumner DR, Weinans H. A decreased subchondral trabecular bone tissue elastic modulus is associated with pre-arthritic cartilage damage. J Orthop Res. 2001; 19:914–918.16. Bobinac D, Spanjol J, Zoricic S, Maric I. Changes in articular cartilage and subchondral bone histomorphometry in osteoarthritic knee joints in humans. Bone. 2003; 32:284–290.17. Ding M, Odgaard A, Hvid I. Changes in the three-dimensional microstructure of human tibial cancellous bone in early osteoarthritis. J Bone Joint Surg Br. 2003; 85:906–912.18. Botter SM, van Osch GJ, Waarsing JH, van der Linden JC, Verhaar JA, Pols HA, et al. Cartilage damage pattern in relation to subchondral plate thickness in a collagenase-induced model of osteoarthritis. Osteoarthritis Cartilage. 2008; 16:506–514.19. Badger AM, Griswold DE, Kapadia R, Blake S, Swift BA, Hoffman SJ, et al. Disease-modifying activity of SB 242235, a selective inhibitor of p38 mitogen-activated protein kinase, in rat adjuvant-induced arthritis. Arthritis Rheum. 2000; 43:175–183.20. Kamibayashi L, Wyss UP, Cooke TD, Zee B. Trabecular microstructure in the medial condyle of the proximal tibia of patients with knee osteoarthritis. Bone. 1995; 17:27–35.21. Patel V, Issever AS, Burghardt A, Laib A, Ries M, Majumdar S. MicroCT evaluation of normal and osteoarthritic bone structure in human knee specimens. J Orthop Res. 2003; 21:6–13.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pathological Characteristics of Monosodium Iodoacetate-Induced Osteoarthritis in Rats
- Anti-osteoarthritis effect of Boswellia serrata gum resin extract in monosodium iodoacetate-induced osteoarthritic Sprague-Dawley rats
- Prevention or treatment of enzyme treated royal jelly on monosodium-iodoacetate-induced osteoarthritis
- Anti-inflammatory effect of egg white-chalcanthite and purple bamboo salts mixture on arthritis induced by monosodium iodoacetate in Sprague-Dawley rats
- Effects of natural eggshell membrane (NEM) on monosodium iodoacetate-induced arthritis in rats