Korean J Urol.
2007 Nov;48(11):1109-1115. 10.4111/kju.2007.48.11.1109.
The Difference in the Prognosis and Characteristics between the Progressive and Primary Muscle-invasive Bladder Cancer Treated with Radical Cystectomy
- Affiliations
-
- 1Department of Urology and Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea. sjhong346@yumc.yonsei.ac.kr
- KMID: 1997085
- DOI: http://doi.org/10.4111/kju.2007.48.11.1109
Abstract
-
PURPOSE: We investigated the difference of the prognosis between progressive and primary muscle-invasive bladder cancer treated with radical cystectomy.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of invasive bladder cancer patients who were treated with radical cystectomy between 1986 and 2004. The patients who underwent progression from superficial cancer to muscle invasive cancer within 3 months, and those who underwent bladder preservation or neoadjuvant therapy were excluded. Fifty progressive muscle-invasive cancer patients (the progressive group) and 173 primary muscle-invasive cancer patients (the primary group) were eligible for this study. Univariate and multivariate analysis were performed to identify the associations between the clinicopathological features and survival, and the characteristics between the two groups were compared with using the chi-square test.
RESULTS
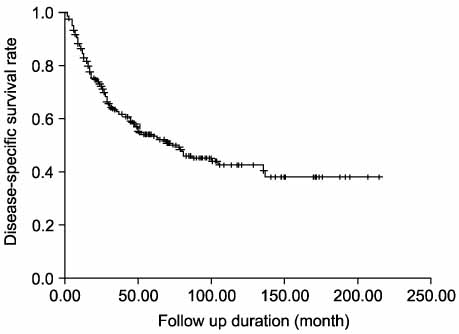
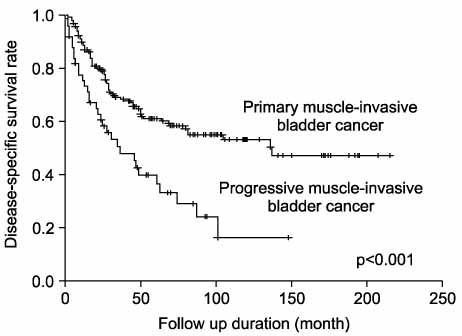
Among the total patients, 102 patients(45.7%) died of cancer. On univariate analysis, age, gender, tumor size, multiplicity, tumor grade and carcinoma in situ did not influence survival(p>0.05). However, the T stage(p<0.001), lymphovascular invasion(p=0.004), and lymph node involvement(p<0.001) had a significant influence on disease-specific survival. Notably, the 5-year disease-specific survival rate for the primary group(61.1%) was significantly higher than that for the progressive group (36.4%)(p<0.001). On multivariate analysis, T stage(p<0.001), lymphovascular invasion(p=0.036), and the progressive disease(p=0.001) were independent prognostic factors. Comparing the characteristics between the two groups, multiplicity was more frequent in the primary group(p=0.029) and nodal involvement was more frequent in the progressive group(p=0.035).
CONCLUSIONS
Progressive muscle-invasive bladder cancer has a poorer prognosis than primary invasive cancer. This poor prognosis is thought to be associated with increased lymph node involvement and micrometastasis in the progressive group.
MeSH Terms
Figure
Cited by 1 articles
-
Pattern of Failure in Bladder Cancer Patients Treated with Radical Cystectomy: Rationale for Adjuvant Radiotherapy
Yong Bae Kim, Sung Joon Hong, Seung Cheol Yang, Jae Ho Cho, Young Deuk Choi, Gwi Eon Kim, Koon Ho Rha, Woong Kyu Han, Nam Hoon Cho, Young Taek Oh
J Korean Med Sci. 2010;25(6):835-840. doi: 10.3346/jkms.2010.25.6.835.
Reference
-
1. Kurth KH, Denis L, Bouffioux C, Sylvester R, Debruyne FM, Pavone-Macaluso M, et al. Factors affecting recurrence and progression in superficial bladder tumours. Eur J Cancer. 1995. 31A:1840–1846.2. Kiemeney LA, Witjes JA, Heijbroek RP, Koper NP, Verbeek AL, Debruyne FM. Members of the Dutch South-East Co-Operative Urological Group. Should random urothelial biopsies be taken from patients with primary superficial bladder cancer? A decision analysis. Br J Urol. 1994. 73:164–171.3. Heney NM, Ahmed S, Flanagan MJ, Frable W, Corder MP, Hafermann MD, et al. Superficial bladder cancer: progression and recurrence. J Urol. 1983. 130:1083–1086.4. Stein JP, Grossfeld GD, Ginsberg DA, Esrig D, Freeman JA, Figueroa AJ, et al. Prognostic markers in bladder cancer: a contemporary review of the literature. J Urol. 1998. 160:645–659.5. Smits G, Schaafsma E, Kiemeney L, Caris C, Debruyne F, Witjes JA. Microstaging of pT1 transitional cell carcinoma of the bladder: identification of subgroups with distinct risks of progression. Urology. 1998. 52:1009–1013.6. Ghoneim MA, El-Mekresh MM, El-Baz MA, El-Attar IA, Ashamallah A. Radical cystectomy for carcinoma of the bladder: critical evaluation of the results in 1,026 cases. J Urol. 1997. 158:393–399.7. Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol. 2001. 19:666–675.8. Yeo JK, Ko YS, Ko YH, Yoon DK. The prognostic difference between the invasive bladder cancer at the initial diagnosis and the invasive bladder cancer progressed from superficial. Korean J Urol. 2002. 43:112–116.9. Schrier BP, Hollander MP, van Rhijn BW, Kiemeney LA, Witjes JA. Prognosis of muscle-invasive bladder cancer: difference between primary and progressive tumours and implications for therapy. Eur Urol. 2004. 45:292–296.10. El-Abbady AA, Shoukry MS, Hanno AG, Younis LK, Abdel-Rahman M. Repeated transurethral resection of recurrent superficial bladder tumors--does it affect the spread and stage of the tumor? Scand J Urol Nephrol. 2002. 36:60–64.11. Brauers A, Buettner R, Jakse G. Second resection and prognosis of primary high risk superficial bladder cancer: is cystectomy often too early? J Urol. 2001. 165:808–810.12. Herr HW. The value of a second transurethral resection in evaluating patients with bladder tumors. J Urol. 1999. 162:74–76.13. Pagano F, Bassi P, Galetti TP, Meneghini A, Milani C, Artibani W, et al. Results of contemporary radical cystectomy for invasive bladder cancer: a clinicopathological study with an emphasis on the inadequacy of the tumor, nodes and metastases classification. J Urol. 1991. 145:45–50.14. Dalbagni G, Herr HW, Reuter VE. Impact of a second transurethral resection on the staging of T1 bladder cancer. Urology. 2002. 60:822–824.15. Zlotta AR, Schulman CC. Biological markers in superficial bladder tumors and their prognostic significance. Urol Clin North Am. 2000. 27:179–189.16. Brake M, Loertzer H, Horsch R, Keller H. Recurrence and progression of stage T1, Grade 3 transitional cell carcinoma of the bladder following intravesical immunotherapy with bacillus Calmette-Guerin. J Urol. 2000. 163:1697–1701.17. Soloway MS, Sofer M, Vaidya A. Contemporary management of stage T1 transitional cell carcinoma of the bladder. J Urol. 2002. 167:1573–1583.18. Herr HW, Sogani PC. Does early cystectomy improve the survival of patients with high risk superficial bladder tumors? J Urol. 2001. 166:1296–1299.19. Dutta SC, Smith JJA, Shappell SB, Coffey CS, Chang SS, Cookson MS. Clinical under staging of high risk nonmuscle invasive urothelial carcinoma treated with radical cystectomy. J Urol. 2001. 166:490–493.20. Gschwend JE, Fair WR, Vieweg J. Radical cystectomy for invasive bladder cancer: contemporary results and remaining controversies. Eur Urol. 2000. 38:121–130.21. Pansadoro V, Emiliozzi P, de Paula F, Scarpone P, Pansadoro A, Sternberg CN. Long-term follow-up of G3T1 transitional cell carcinoma of the bladder treated with intravesical bacille Calmette-Guerin: 18-year experience. Urology. 2002. 59:227–231.22. Sylvester RJ, van der Meijden AP, Lamm DL. Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. J Urol. 2002. 168:1964–1970.23. Esrig D, Freeman JA, Stein JP, Skinner DG. Early cystectomy for clinical stage T1 transitional cell carcinoma of the bladder. Semin Urol Oncol. 1997. 15:154–160.24. Amling CL, Thrasher JB, Frazier HA, Dodge RK, Robertson JE, Paulson DF. Radical cystectomy for stages Ta, Tis and T1 transitional cell carcinoma of the bladder. J Urol. 1994. 151:31–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Significance of the Presence of Proper Muscle in the Resected Specimens of Primary T1G3 Bladder Cancer
- Current Evidence for the Treatment of Bladder Cancer
- Does Transurethral Resection Affect the Results of Computed Tomography in the Clinical Staging of Invasive Bladder Cancer?
- Robot-Assisted Laparoscopic Radical Cystectomy
- Laparoscopic Partial Cystectomy for Adenocarcinoma of the Bladder