Korean J Urol.
2012 Jan;53(1):23-28. 10.4111/kju.2012.53.1.23.
Impact of Changing Trends in Medical Therapy on Surgery for Benign Prostatic Hyperplasia Over Two Decades
- Affiliations
-
- 1Department of Urology, Chung-Ang University College of Medicine, Seoul, Korea. caucih@cau.ac.kr
- 2Department of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 1988819
- DOI: http://doi.org/10.4111/kju.2012.53.1.23
Abstract
- PURPOSE
Following the introduction of medical therapy for benign prostatic hyperplasia (BPH), we determined the effect of the change in trends in medical therapy on the indication and outcome of surgical intervention for BPH.
MATERIALS AND METHODS
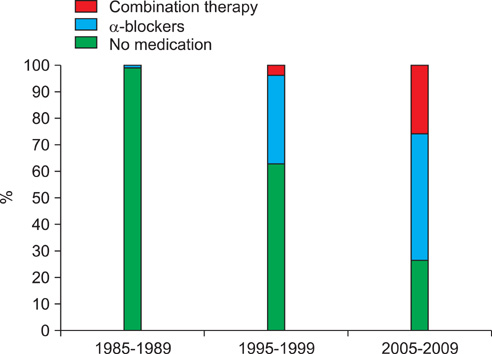
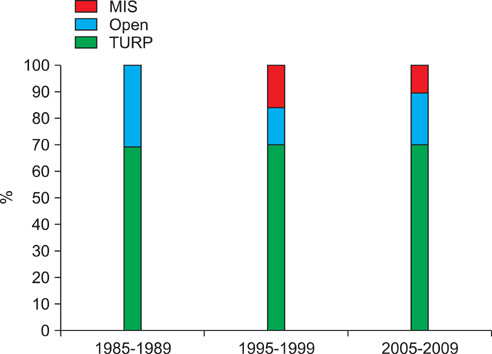
We compared the basic characteristics of, weight of resected tissue of, transfusions in, and postoperative complications of patients who underwent surgery between 1985 and 1989 (before the advent of medical therapy for BPH), between 1995 and 1999 (when medical therapy was developed and became widely used as alternative treatment), and between 2005 and 2009 (when medical therapy superseded surgical intervention to become first-line treatment and when combination therapy became widely adopted).
RESULTS
At our institution, the mean age and BMI of patients increased over the past two decades (p<0.001). Hypertension, operation history, and other comorbidities also increased significantly (p<0.001, p=0.005, and p<0.001, respectively). The indications for surgery in 1985 to 1989, 1995 to 1999, and 2005 to 2009 were as follows: acute urinary retention in 34.7%, 20.2%, and 15.1% of patients and symptomatic deterioration in 61.1%, 72.3%, and 73.0% of patients, respectively. Prostate volume and the weight of resected tissue increased from 34.4+/-14.5 ml to 61.3+/-32.4 ml and from 7.2+/-6.4 g to 10.8+/-7.6 g, respectively, over two decades. Patients who underwent surgery in 2005 to 2009 had their catheters removed earlier (p<0.001). Secondary hemorrhage within four postoperative weeks and repeat transurethral resection of the prostate within 1 year decreased significantly (p=0.03 and p=0.003, respectively). No statistically significant change in impaired detrusor contractility was found (p=0.523).
CONCLUSIONS
Although patients who underwent surgery were older after widespread use of medical therapy for BPH, advancements in surgical techniques have benefitted these patients.
MeSH Terms
Figure
Cited by 1 articles
-
Thermo-expandable prostatic stents for bladder outlet obstruction in the frail and elderly population: An underutilized procedure?
Kapil Sethi, Michael Bozin, Tebogo Jabane, Richard McMullin, David Cook, Rob Forsyth, Lachlan Dodds, Lydia Johns Putra
Investig Clin Urol. 2017;58(6):447-452. doi: 10.4111/icu.2017.58.6.447.
Reference
-
1. Flanigan RC, Reda DJ, Wasson JH, Anderson RJ, Abdellatif M, Bruskewitz RC. 5-year outcome of surgical resection and watchful waiting for men with moderately symptomatic benign prostatic hyperplasia: a Department of Veterans Affairs cooperative study. J Urol. 1998. 160:12–16.2. Reich O, Gratzke C, Stief CG. Techniques and long-term results of surgical procedures for BPH. Eur Urol. 2006. 49:970–978.3. Chung BH, Yang KM, Hong SJ. Meta-analysis of alpha receptor antagosist for benign prostatic hyperplasia from papers that were published in Korea. Korean J Urol. 2005. 46:252–258.4. Lepor H, Auerbach S, Puras-Baez A, Narayan P, Soloway M, Lowe F, et al. A randomized, placebo-controlled multicenter study of the efficacy and safety of terazosin in the treatment of benign prostatic hyperplasia. J Urol. 1992. 148:1467–1474.5. McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003. 349:2387–2398.6. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.7. Clifford GM, Farmer RD. Medical therapy for benign prostatic hyperplasia: a review of the literature. Eur Urol. 2000. 38:2–19.8. Chang HS, Park CH, Kim CI. Comparison of the long term effect of alpha-blocker only and 5-alpha reductase inhibitor combination treatment on acute urinary retention and prostatic surgery for patients with benign prostatic hyperplasia. Korean J Urol. 2006. 47:7–12.9. Izard J, Nickel JC. Impact of medical therapy on transurethral resection of the prostate: two decades of change. BJU Int. 2010. 108:89–93.10. Vela-Navarrete R, Gonzalez-Enguita C, Garcia-Cardoso JV, Manzarbeitia F, Sarasa-Corral JL, Granizo JJ. The impact of medical therapy on surgery for benign prostatic hyperplasia: a study comparing changes in a decade (1992-2002). BJU Int. 2005. 96:1045–1048.11. Kuczmarski RJ, Carroll MD, Flegal KM, Troiano RP. Varying body mass index cutoff points to describe overweight prevalence among U.S. adults: NHANES III (1988 to 1994). Obes Res. 1997. 5:542–548.12. Barreto SM, Passos VM, Firmo JO, Guerra HL, Vidigal PG, Lima-Costa MF. Hypertension and clustering of cardiovascular risk factors in a community in Southeast Brazil--The Bambui Health and Ageing Study. Arq Bras Cardiol. 2001. 77:576–581.13. Han KS, Hong SJ, Chung BH. Changing trends in the management of bengin prostatic hyperplasia during recent 5 years. Korean J Urol. 2005. 46:458–462.14. Shin YS, Park JK. Changes in surgical strategy for patients with benign prostatic hyperplasia: 12-year single-center experience. Korean J Urol. 2011. 52:189–193.15. Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008. 180:246–249.16. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989. 141:243–247.17. Starkman JS, Santucci RA. Comparison of bipolar transurethral resection of the prostate with standard transurethral prostatectomy: shorter stay, earlier catheter removal and fewer complications. BJU Int. 2005. 95:69–71.18. Saito M, Ohmura M, Kondo A. Restoration of rat bladder function following release of short- and long-term partial outflow obstruction. Urol Res. 1997. 25:193–197.19. Boyle P, Roehrborn C, Harkaway R, Logie J, de la Rosette J, Emberton M. 5-Alpha reductase inhibition provides superior benefits to alpha blockade by preventing AUR and BPH-related surgery. Eur Urol. 2004. 45:620–626.20. Wasson JH, Bubolz TA, Lu-Yao GL, Walker-Corkery E, Hammond CS, Barry MJ. Transurethral resection of the prostate among medicare beneficiaries: 1984 to 1997. For the Patient Outcomes Research Team for Prostatic Diseases. J Urol. 2000. 164:1212–1215.21. Borth CS, Beiko DT, Nickel JC. Impact of medical therapy on transurethral resection of the prostate: a decade of change. Urology. 2001. 57:1082–1085.22. Kim TS, Choi S, Rhew HY, Ahn JH, Jang JH, Cho MH. Comparative study on the treatment outcome and safety of TURP, ILC, TUNA and TEAP for patients with benign prostatic hyperplasia. Korean J Urol. 2006. 47:13–19.23. Kwon JS, Lee JW, Lee SW, Choi HY, Moon HS. Comparison of effectiveness of monopolar and bipolar transurethral resection of the prostate and open prostatectomy in large benign prostatic hyperplasia. Korean J Urol. 2011. 52:269–273.24. Tan AH, Gilling PJ. Lasers in the treatment of benign prostatic hyperplasia: an update. Curr Opin Urol. 2005. 15:55–58.25. Bhansali M, Patankar S, Dobhada S, Khaladkar S. Management of large (>60 g) prostate gland: PlasmaKinetic Superpulse (bipolar) versus conventional (monopolar) transurethral resection of the prostate. J Endourol. 2009. 23:141–145.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Prominently Large Glans penis as a Possible sign of Benign Prostatic Hyperplasia
- Histopathologic Study of non-Cancerous Lesion of the Prostate
- Medical Management for Benign Prostatic Hyperplasia
- The Evolution of KTP Laser Vaporization of the Prostate
- The Effects of Abdominal Obesity on the Increased Prevalence Rate of Hypertension and Diabetes Mellitus in Benign Prostatic Hyperplasia Patients