The Survey about the Degree of Damage of Radiation-Protective Shields in Operation Room
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University Medical Center, Seoul, Korea. painfree@kuh.ac.kr
- 2Department of Anesthesiology and Pain Medicine, Jeju National University Hospital, Jeju, Korea.
- KMID: 1978658
- DOI: http://doi.org/10.3344/kjp.2013.26.2.142
Abstract
- BACKGROUND
Medical doctors who perform C-arm fluoroscopy-guided procedures are exposed to X-ray radiation. Therefore, radiation-protective shields are recommended to protect these doctors from radiation. For the past several years, these protective shields have sometimes been used without regular inspection. The aim of this study was to investigate the degree of damage to radiation-protective shields in the operating room.
METHODS
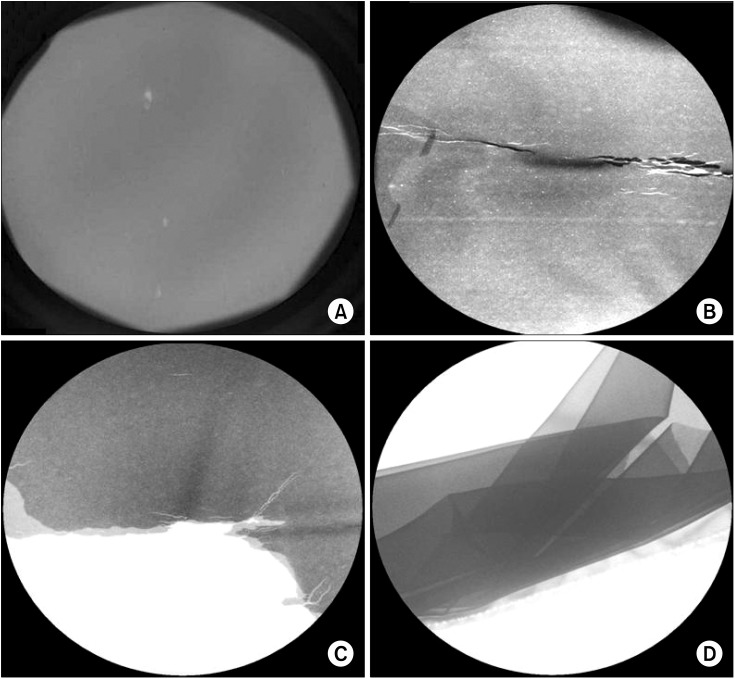
This study investigated 98 radiation-protective shields in the operation rooms of Konkuk University Medical Center and Jeju National University Hospital. We examined whether these shields were damaged or not with the unaided eye and by fluoroscopy.
RESULTS
There were seventy-one aprons and twenty-seven thyroid protectors in the two university hospitals. Fourteen aprons (19.7%) were damaged, whereas no thyroid protectors (0%) were. Of the twenty-six aprons, which have been used since 2005, eleven (42.3%) were damaged. Of the ten aprons, which have been used since 2008, none (0%) was damaged. Of the twenty-three aprons that have been used since 2009, two (8.7%) of them were damaged. Of the eight aprons used since 2010, one (12.3%) was damaged. Of the four aprons used since 2011, none (0%) of them were damaged. The most common site of damage to the radiation-protective shields was at the waist of the aprons (51%).
CONCLUSIONS
As a result, aprons that have been used for a long period of time can have a higher risk of damage. Radiation-protective shields should be inspected regularly and exchanged for new products for the safety of medical workers.
Figure
Cited by 7 articles
-
Radiation Safety for Pain Physicians: Technique or Equipment
Jae Hang Shim
Korean J Pain. 2014;27(2):101-102. doi: 10.3344/kjp.2014.27.2.101.The Radiation Exposure of Radiographer Related to the Location in C-arm Fluoroscopy-guided Pain Interventions
Young Jae Chang, Ah Na Kim, In Su Oh, Nam Sik Woo, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2014;27(2):162-167. doi: 10.3344/kjp.2014.27.2.162.How Effective Are Radiation Reducing Gloves in C-arm Fluoroscopy-guided Pain Interventions?
Ah Na Kim, Young Jae Chang, Bo Kyung Cheon, Jae Hun Kim
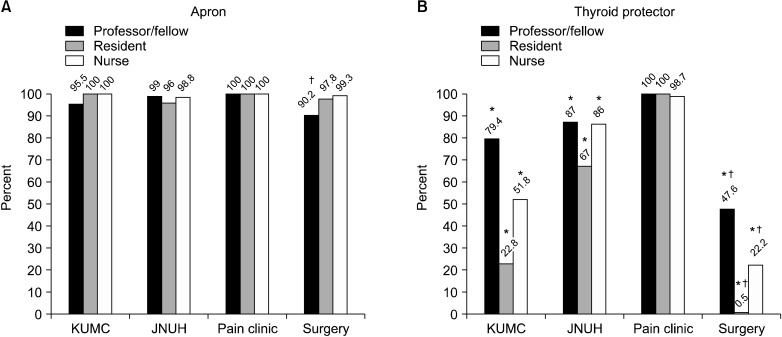
Korean J Pain. 2014;27(2):145-151. doi: 10.3344/kjp.2014.27.2.145.The radiation safety education and the pain physicians' efforts to reduce radiation exposure
Tae Hee Kim, Seung Wan Hong, Nam Sik Woo, Hae Kyoung Kim, Jae Hun Kim
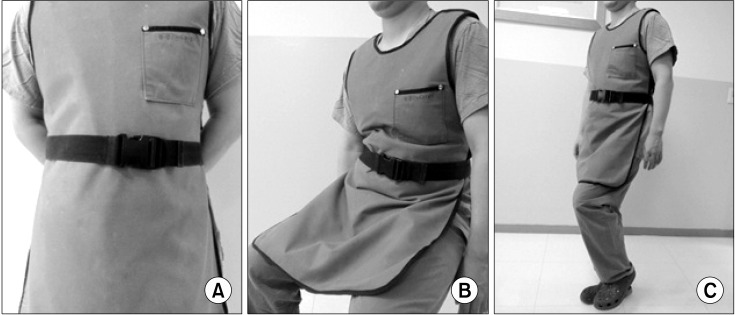
Korean J Pain. 2017;30(2):104-115. doi: 10.3344/kjp.2017.30.2.104.Three principles for radiation safety: time, distance, and shielding
Jae Hun Kim
Korean J Pain. 2018;31(3):145-146. doi: 10.3344/kjp.2018.31.3.145.Radiation safety: a focus on lead aprons and thyroid shields in interventional pain management
Bo Kyung Cheon, Cho Long Kim, Ka Ram Kim, Min Hye Kang, Jeong Ae Lim, Nam Sik Woo, Ka Young Rhee, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2018;31(4):244-252. doi: 10.3344/kjp.2018.31.4.244.Radiation safety for pain physicians: principles and recommendations
Sewon Park, Minjung Kim, Jae Hun Kim
Korean J Pain. 2022;35(2):129-139. doi: 10.3344/kjp.2022.35.2.129.
Reference
-
1. Kim TW, Jung JH, Jeon HJ, Yoon KB, Yoon DM. Radiation exposure to physicians during interventional pain procedures. Korean J Pain. 2010; 23:24–27. PMID: 20552069.
Article2. Le Heron J, Padovani R, Smith I, Czarwinski R. Radiation protection of medical staff. Eur J Radiol. 2010; 76:20–23. PMID: 20656429.
Article4. Mroz TE, Yamashita T, Davros WJ, Lieberman IH. Radiation exposure to the surgeon and the patient during kyphoplasty. J Spinal Disord Tech. 2008; 21:96–100. PMID: 18391712.
Article5. Cousins C, Sharp C. Medical interventional procedures-reducing the radiation risks. Clin Radiol. 2004; 59:468–473. PMID: 15145716.
Article6. Shope TB. Radiation-induced skin injuries from fluoroscopy. Radiographics. 1996; 16:1195–1199. PMID: 8888398.
Article7. Schueler BA. Operator shielding: how and why. Tech Vasc Interv Radiol. 2010; 13:167–171. PMID: 20723831.
Article8. Yaffe MJ, Mawdsley GE, Lilley M, Servant R, Reh G. Composite materials for x-ray protection. Health Phys. 1991; 60:661–664. PMID: 2019497.
Article9. Poletti JL, McLean D. The effect of source to image-receptor distance on effective dose for some common X-ray projections. Br J Radiol. 2005; 78:810–815. PMID: 16110102.
Article10. Botwin KP, Freeman ED, Gruber RD, Torres-Rames FM, Bouchtas CG, Sanelli JT, et al. Radiation exposure to the physician performing fluoroscopically guided caudal epidural steroid injections. Pain Physician. 2001; 4:343–348. PMID: 16902680.11. Hellawell GO, Mutch SJ, Thevendran G, Wells E, Morgan RJ. Radiation exposure and the urologist: what are the risks? J Urol. 2005; 174:948–952. PMID: 16094003.
Article12. Manchikanti L, Cash KA, Moss TL, Pampati V. Radiation exposure to the physician in interventional pain management. Pain Physician. 2002; 5:385–393. PMID: 16886017.
Article13. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007; 37:1–332.14. Miller DL, Vañó E, Bartal G, Balter S, Dixon R, Padovani R, et al. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. J Vasc Interv Radiol. 2010; 21:607–615. PMID: 20430294.
Article15. Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005; 13:69–76. PMID: 15712984.
Article16. Powys R, Robinson J, Kench PL, Ryan J, Brennan PC. Strict X-ray beam collimation for facial bones examination can increase lens exposure. Br J Radiol. 2012; 85:e497–e505. PMID: 22374279.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiation safety: a focus on lead aprons and thyroid shields in interventional pain management
- A Survey of the Radiation Exposure Protection of Health Care Providers during Endoscopic Retrograde Cholangiopancreatography in Korea
- Acute Phase Retinal Phototoxicity Induced by Blue Fluorescent Light
- Radiation exposure in diagnostic radiology
- The protective effects of trace elements against side effects induced by ionizing radiation