Cancer Res Treat.
2012 Sep;44(3):187-194.
Interval between Surgery and Radiation Therapy Is an Important Prognostic Factor in Treatment of Rectal Cancer
- Affiliations
-
- 1Department of Radiation Oncology, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. jhkim@dsmc.or.kr
- 2Department of General Surgery, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
Abstract
- PURPOSE
The purpose of this study is to evaluate survival and prognostic factors for rectal cancer, including interval between surgery and radiation therapy after surgery, radiation therapy, and chemotherapy.
MATERIALS AND METHODS
We conducted a retrospective study of 153 patients with rectal cancer who were treated with surgery, radiotherapy with/without chemotherapy at Keimyung University Dongsan Medical Center from January, 1988 to December, 2005. The study included 89 males and 64 females, with a median age of 56 years (range, 23 to 81 years). Tumor, node and metastasis (TNM) was I in 23 patients, II in 39, and III in 91. Radiation therapy was performed on pelvic fields using a median dose of 54 Gy five days per week, 1.8 Gy once per day. Ninety two patients were treated with radiotherapy, 43 with concurrent chemo-radiation therapy and 18 with sequential therapy after surgery. The median follow-up period was 52 months (range, 4 to 272 months). The interval between surgery and radiation was 1-25 weeks (median, 5 weeks).
RESULTS
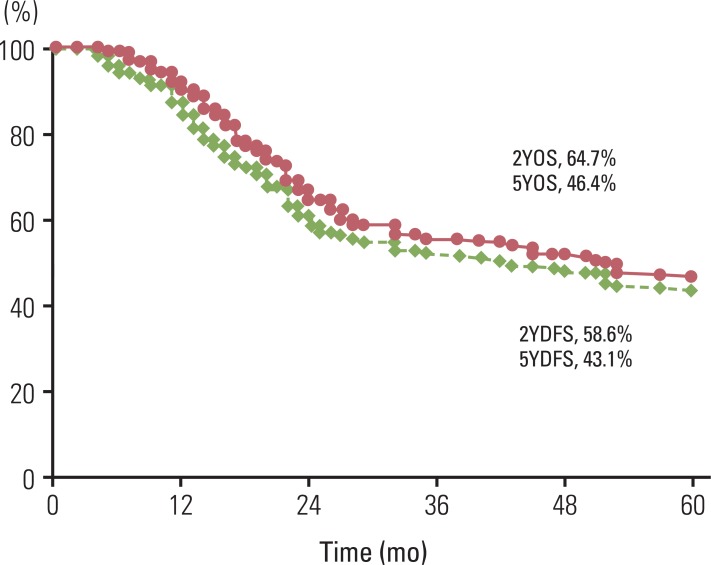
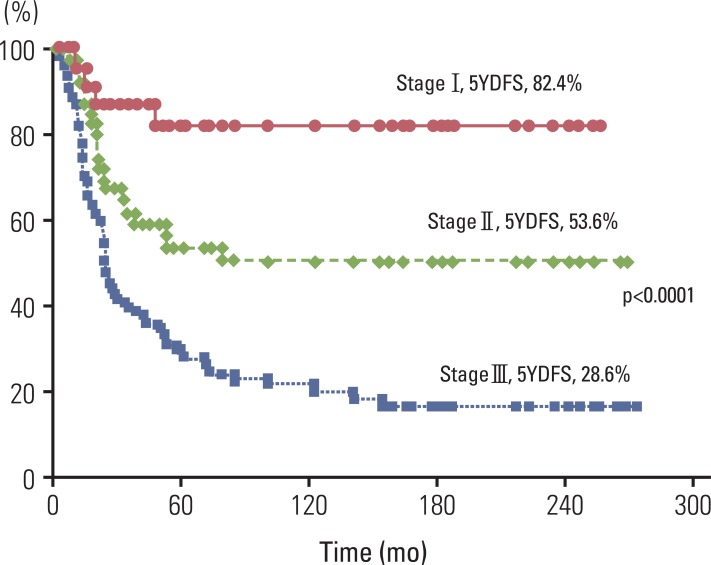
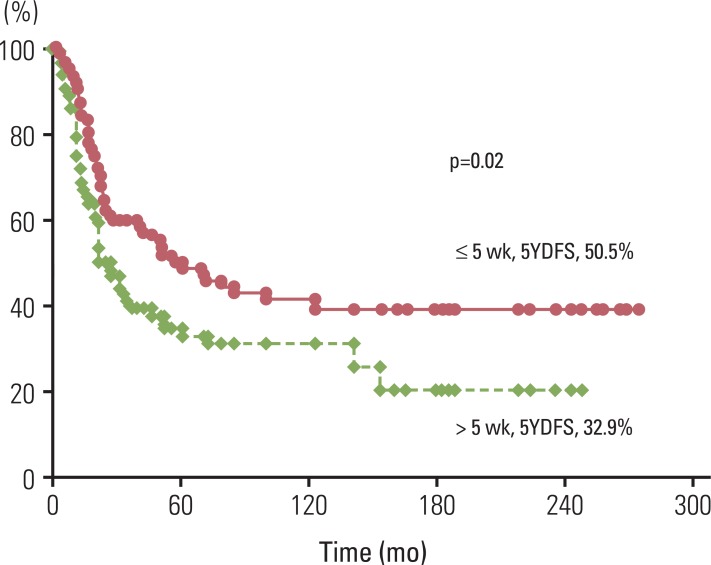
Two-year and five-year overall survival rate was 64.7% and 46.4%, respectively. Two-year and five-year disease-free-survival (DFS) rate was 58.6% and 43.1%, respectively. Median DFS was 39 months. Loco-regional failure was evident in 10.5% of patients, 8.4% had distant metastasis, and 9.2% had both. In multivariate analysis, TNM stage and interval between surgery and radiation therapy (< or =5 weeks vs. >5 weeks; 95% confidence interval, 1.276 to 2.877; hazard ratio, 1.916; p=0.002) were significant prognostic factors of DFS.
CONCLUSION
Survival rates for rectal cancer after surgery, chemotherapy, and radiation therapy were similar to those reported in previous studies. Starting radiation therapy as soon as possible after surgery, especially within the first five weeks after surgery, is suggested.
MeSH Terms
Figure
Reference
-
1. Balslev I, Pedersen M, Teglbjaerg PS, Hanberg-Soerensen F, Bone J, Jacobsen NO, et al. Postoperative radiotherapy in Dukes' B and C carcinoma of the rectum and rectosigmoid: a randomized multicenter study. Cancer. 1986; 58:22–28. PMID: 3518912.
Article2. Mohiuddin M, Czito BG, Willett CG. Halperin EC, Perez CA, Brady LW, editors. Colon and rectum. Perez and Brady's principles and practice of radiation oncology. 2008. 5th ed. Philadelphia: Lippincott Williams and Wilkins;p. 1366–1382.3. Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet. 2001; 358:1291–1304. PMID: 11684209.4. Krook JE, Moertel CG, Gunderson LL, Wieand HS, Collins RT, Beart RW, et al. Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med. 1991; 324:709–715. PMID: 1997835.
Article5. Wolmark N, Wieand HS, Hyams DM, Colangelo L, Dimitrov NV, Romond EH, et al. Randomized trial of postoperative adjuvant chemotherapy with or without radiotherapy for carcinoma of the rectum: National Surgical Adjuvant Breast and Bowel Project Protocol R-02. J Natl Cancer Inst. 2000; 92:388–396. PMID: 10699069.
Article6. Fisher B, Wolmark N, Rockette H, Redmond C, Deutsch M, Wickerham DL, et al. Postoperative adjuvant chemotherapy or radiation therapy for rectal cancer: results from NSABP protocol R-01. J Natl Cancer Inst. 1988; 80:21–29. PMID: 3276900.7. NIH consensus conference. Adjuvant therapy for patients with colon and rectal cancer. JAMA. 1990; 264:1444–1450. PMID: 2202842.8. O'Connell MJ, Martenson JA, Wieand HS, Krook JE, Macdonald JS, Haller DG, et al. Improving adjuvant therapy for rectal cancer by combining protracted-infusion fluorouracil with radiation therapy after curative surgery. N Engl J Med. 1994; 331:502–507. PMID: 8041415.9. Vikram B, Farr HW. Adjuvant radiation therapy in locally advanced head and neck cancer. CA Cancer J Clin. 1983; 33:134–138. PMID: 6404520.
Article10. Douglass HO Jr, Moertel CG, Mayer RJ, Thomas PR, Lindblad AS, Mittleman A, et al. Survival after postoperative combination treatment of rectal cancer. N Engl J Med. 1986; 315:1294–1295. PMID: 3773947.
Article11. Gall FP, Hermanek P. Update of the German experience with local excision of rectal cancer. Surg Oncol Clin N Am. 1992; 1:99–109.
Article12. Nascimbeni R, Burgart LJ, Nivatvongs S, Larson DR. Risk of lymph node metastasis in T1 carcinoma of the colon and rectum. Dis Colon Rectum. 2002; 45:200–206. PMID: 11852333.
Article13. Gastrointestinal Tumor Study Group. Prolongation of the disease-free interval in surgically treated rectal carcinoma. N Engl J Med. 1985; 312:1465–1472. PMID: 2859523.14. Tepper JE, O'Connell MJ, Petroni GR, Hollis D, Cooke E, Benson AB 3rd, et al. Adjuvant postoperative fluorouracil-modulated chemotherapy combined with pelvic radiation therapy for rectal cancer: initial results of intergroup 0114. J Clin Oncol. 1997; 15:2030–2039. PMID: 9164215.
Article15. Kim JS, Kim NK, Min BS, Hur H, Ahn JB, Keum KC. Adjuvant radiotherapy following total mesorectal excision for stage IIA rectal cancer: is it beneficial? Int J Colorectal Dis. 2010; 25:1103–1110. PMID: 20544208.
Article16. Moody JS, Sawrie SM, Kozak KR, Plastaras JP, Howard G, Bonner JA. Stage-specific survival differences associated with postoperative radiotherapy for gastrointestinal cancers. J Gastrointest Cancer. 2008; 39:86–99. PMID: 19294536.
Article17. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al. AJCC cancer staging manual. 2002. 6th ed. New York: Springer-Verlag.18. Schild SE, Martenson JA Jr, Gunderson LL, Ilstrup DM, Berg KK, O'Connell MJ, et al. Postoperative adjuvant therapy of rectal cancer: an analysis of disease control, survival, and prognostic factors. Int J Radiat Oncol Biol Phys. 1989; 17:55–62. PMID: 2745208.
Article19. Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton SR, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000; 124:979–994. PMID: 10888773.20. Crucitti F, Sofo L, Doglietto GB, Bellantone R, Ratto C, Bossola M, et al. Prognostic factors in colorectal cancer: current status and new trends. J Surg Oncol Suppl. 1991; 2:76–82. PMID: 1892535.
Article21. de Campos-Lobato LF, Geisler DP, da Luz Moreira A, Stocchi L, Dietz D, Kalady MF. Neoadjuvant therapy for rectal cancer: the impact of longer interval between chemoradiation and surgery. J Gastrointest Surg. 2011; 15:444–450. PMID: 21140237.
Article22. Tulchinsky H, Shmueli E, Figer A, Klausner JM, Rabau M. An interval >7 weeks between neoadjuvant therapy and surgery improves pathologic complete response and disease-free survival in patients with locally advanced rectal cancer. Ann Surg Oncol. 2008; 15:2661–2667. PMID: 18389322.23. Halperin EC, Perez CA, Brady LW. Halperin EC, Perez CA, Brady LW, editors. The discipline of radiation oncology. Perez and Brady's principles and practice of radiation oncology. 2008. 5th ed. Philadelphia: Lippincott Williams and Wilkins;p. 48–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Impact of Carcinoembryonic Antigen Levels in Rectal Cancer Patients Who Had Received Neoadjuvant Chemoradiotherapy
- Radiation Therapy for Rectal Cancer
- Total Mesorectal Excision: Is It a Valid Prognostic Factor for Recurrence?
- TNM Staging, Molecular Staging and Prognostic Factors of Rectal Cancer
- The Results of Postoperative Radiation Therapy in the Rectal Cancer