Ann Rehabil Med.
2011 Aug;35(4):529-534. 10.5535/arm.2011.35.4.529.
Evaluation of Elbow Stretch Reflex Using a Portable Hand-driven Isokinetic System in Normal Adults
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Institute for Medical Sciences, Chonbuk National University Medical School, Research Institute of Clinical Medicine, Chonbuk National University Hospital, Jeonju 561-180, Korea. credomea@naver.com
- 2Division of Electronics and Information Engineering, Chonbuk National University, Jeonju 561-180, Korea.
- KMID: 1971719
- DOI: http://doi.org/10.5535/arm.2011.35.4.529
Abstract
OBJECTIVE
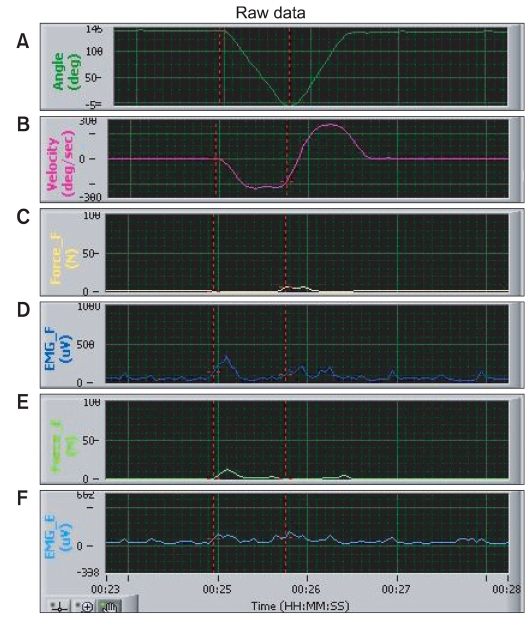
To evaluate normal healthy persons without spasticity to observe normal findings of the elbow stretch reflex using a newly developed, portable, hand-driven spasticity-measuring system. METHOD: Thirty normal persons without any disease involving the central or peripheral nervous system were enrolled in this study. The portable hand-driven isokinetic system is able to measure the joint angle, angular velocity, electromyographic (EMG) signals, and torque during elbow passive extension-flexion. One set of 10 passive elbow extension and flexion movements was performed for data acquisition at each angular velocity, including 60, 90, 120, 150 and 180 degrees per second (degrees/sec). Electromyographic data were collected from the biceps brachii and the triceps brachii. Torque data were collected from sensors around the wrist.
RESULTS
We were able to detect EMG activity and torque in all subjects by using the new portable hand-driven isokinetic system. EMG activity and torque increased with incremental increase of angular velocities. The joint angle of maximal EMG activity according to different angular velocities did not show any significant difference (116degrees-127degrees in elbow extension and 37degrees-66degrees in elbow flexion). The joint angles of maximal torque according to different angular velocities were not significantly different either.
CONCLUSION
Using the portable hand-driven isokinetic system on the elbows of normal subjects, we were able to obtain expected results. By considering our normal findings of the elbow stretch reflex using this system, we propose that the various aspects of spasticity-related data can be measured successfully.
Keyword
Figure
Reference
-
1. Ashworth B. Preliminary trial of carisprodol in multiple sclerosis. Practitioner. 1964; 192:540–542. PMID: 14143329.2. Gregson JM, Leathley M, Moore AP, Sharma AK, Smith TL, Watkins CL. Reliability of the Tone Assessment Scale and the modified Ashworth scale as clinical tools for assessing poststroke spasticity. Arch Phys Med Rehabil. 1999; 80:1013–1016. PMID: 10489001.
Article3. Gregson JM, Leathley MJ, Moore AP, Smith TL, Sharma AK, Watkins CL. Reliability of measurements of muscle tone and muscle power in stroke patients. Age Ageing. 2000; 29:223–228. PMID: 10855904.4. Fowler EG, Nzigwe AI, Ho TW. Sensitivity of the pendulum test for assessing spasticity in persons with cerebral palsy. Dev Med Child Neurol. 2000; 42:182–189. PMID: 10755458.
Article5. Alibiglou L, Rymer WZ, Harvey RL, Mirbagheri MM. The relation between Ashworth scores and neuromechanical measurements of spasticity following stroke. J NeuroEng Rehabil. 2008; 5:18–31. PMID: 18627628.
Article6. Kohan AH, Abootalebi S, Khoshnevisan A, Rahgozar M. Comparison of modified Ashworth scale and Hoffmann reflex in study of spasticity. Acta Med Iran. 2010; 48:154–157. PMID: 21137650.7. Seo JH, Han SH, Kim KS, Song CG, Ko MH, Park SH. Evaluation of stretch reflex threshold on stroke patients using the new portable spasticity-measuring system. J Korean Assoc EMG-Electrodiagn Med. 2009; 11:85–91.8. Sinkjaer T, Toft E, Andreassen S, Hornemann BC. Muscle stiffness in human ankle dorsiflexors: intrinsic and reflex components. J Neurophysiol. 1988; 60:1110–1121. PMID: 3171659.
Article9. Bucho I, Anastasievich R. Activity of fusimotor neurons during reflex muscle contraction. Neirofiziologiia. 1984; 16:630–637. PMID: 6514061.10. Nichols TR, Houk JC. Improvement in linearity and regulation of stiffness that results from actions of stretch reflex. J Neurophysiol. 1976; 39:119–142. PMID: 1249597.
Article11. Simon BN, Verstraete MC, Reisberg S, Mulavara AP. Torque production vs muscle activity during knee flexion extension. IEEE Eng Med Biol Mag. 1994; 1:382–383.12. Pisano F, Miscio G, Colombo R, Pinelli P. Quantitative evaluation of normal muscle tone. J Neurol Sci. 1996; 135:168–172. PMID: 8867074.
Article13. Lee SJ, Kwon BS, Chung SY. The significance of stretch reflex threshold speed in quantitative assessment of spasticity. J Korean Acad Rehabil Med. 2000; 24:208–214.14. Neilson PD, McCaughey J. Effect of contraction level and magnitude of stretch on tonic stretch reflex transmission characteristics. J Neurol Neurosurg Psychiatry. 1981; 44:1007–1012. PMID: 6278094.
Article15. Pandyan AD, Price CI, Rodgers H, Barnes MP, Johnson GR. Biomechanical examination of a commonly used measure of spasticity. Clin Biomech (Bristol, Avon). 2001; 16:859–865.
Article16. Lee SJ, Kwon BS, Park ST. The assessment of spasticity using isokinetic eccentric torque measurement. J Korean Acad Rehabil Med. 1999; 23:828–834.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Assessment of Spasticity Using Isokinetic Eccentric Torque Measurement
- Quantitative Analysis of Tendon Reflexes of Upper Extremities in Normal Volunteers
- The Effects of Jendrassik Maneuver on the T-reflex and the H-reflex of Soleus Muscle
- Activation of Human Stretch Reflex by Experimental Muscle Pain
- The Quantitative Assessment of Ankle Plantar Flexor Muscle Tone