J Cerebrovasc Endovasc Neurosurg.
2015 Mar;17(1):36-42. 10.7461/jcen.2015.17.1.36.
Delayed Perilesional Ischemic Stroke after Gamma-knife Radiosurgery for Unruptured Deep Arteriovenous Malformation: Two Case Reports of Radiation-induced Small Artery Injury as Possible Cause
- Affiliations
-
- 1Department of Neurosurgery, Kyungpook National University Hospital, Daegu, Korea. kdhdock@hotmail.com
- 2Department of Radiology, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 1963148
- DOI: http://doi.org/10.7461/jcen.2015.17.1.36
Abstract
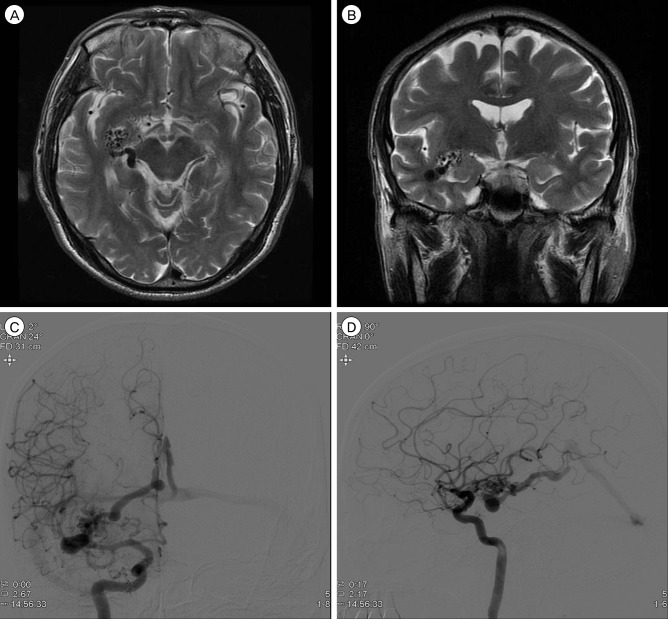
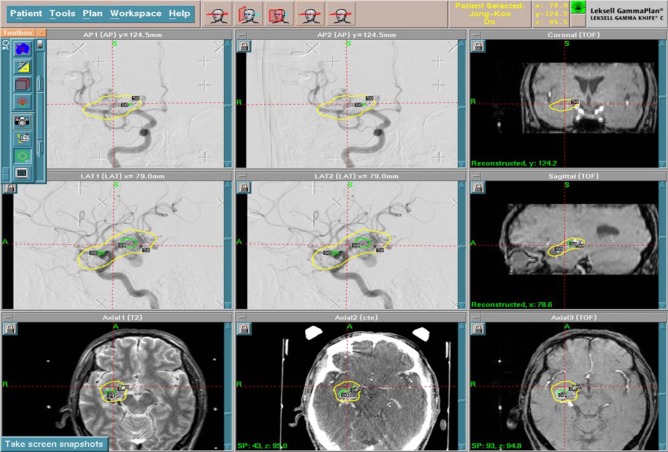
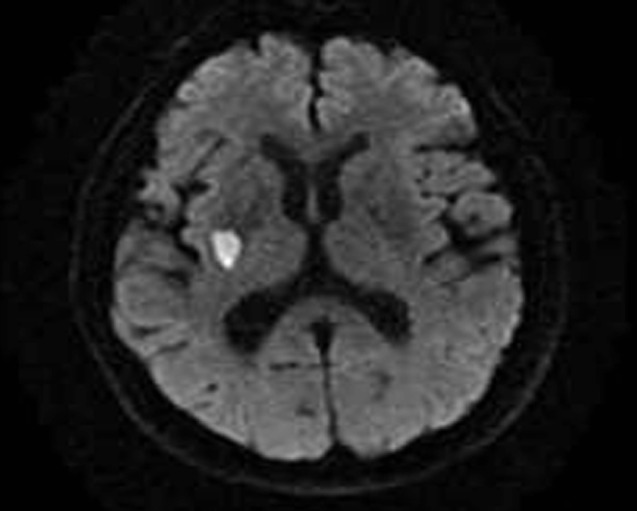
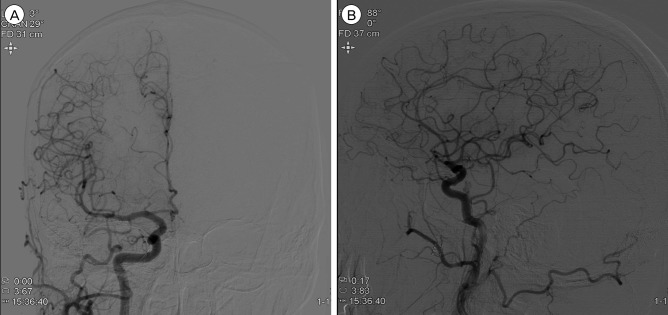
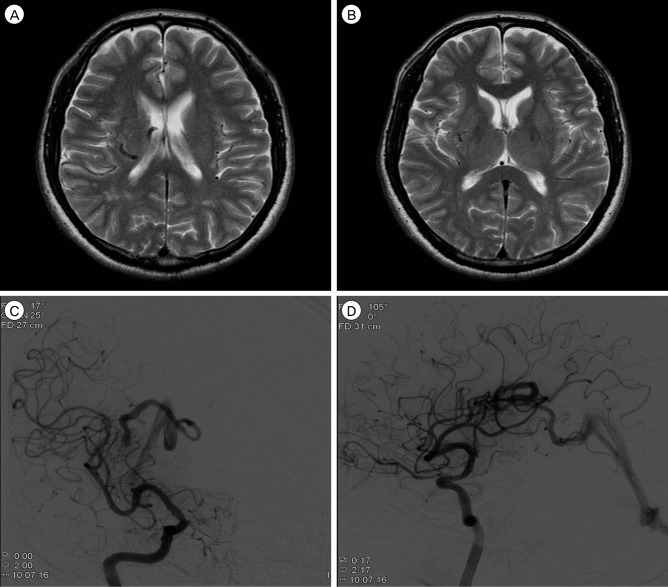
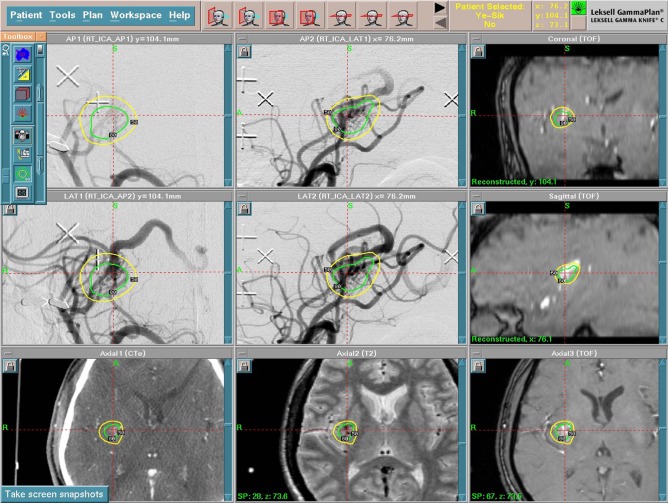
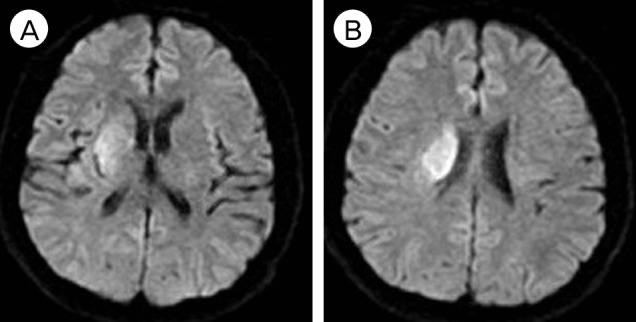
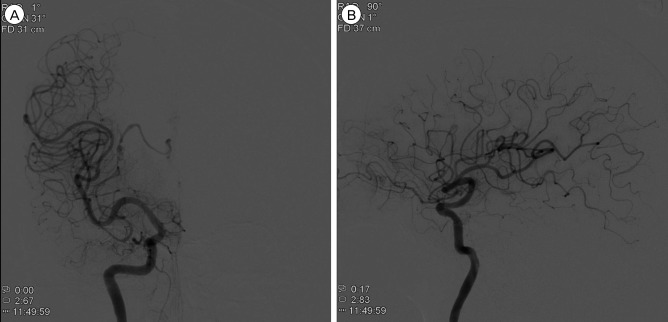
- Radiation-induced vasculopathy is a rare occurrence, however, it is one of the most serious complications that can occur after gamma-knife radiosurgery (GKRS). The authors present two cases of incidentally found deep cerebral arteriovenous malformation (AVM), which were treated by GKRS, where subsequently there occurred delayed-onset cerebral infarction (11 and 17 months after GKRS) at an area adjacent to the AVM. In both cases, perforators of the M1 segment of the middle cerebral artery were included in the radiation field and delayed injury to these is suggested to be the mechanism of the ischemic event.
Keyword
MeSH Terms
Figure
Reference
-
1. Betti OO, Munari C, Rosler R. Stereotactic radiosurgery with the linear accelerator: treatment of arteriovenous malformations. Neurosurgery. 1989; 3. 24(3):311–321. PMID: 2648180.
Article2. Chiou TS, Tsai CH, Lee YH. Unilateral Holmes tremor and focal dystonia after Gamma Knife surgery. J Neurosurg. 2006; 12. 105(Suppl):235–237. PMID: 18503362.
Article3. Gross BA, Ropper AE, Du R. Vascular complications of stereotactic radiosurgery for arteriovenous malformations. Clin Neurol Neurosurg. 2013; 6. 115(6):713–717. PMID: 22910397.
Article4. Lim YJ, Leem W, Park JT, Kim TS, Rhee BA, Kim GK. Cerebral infarction with ICA occlusion after Gamma Knife radiosurgery for pituitary adenoma: A case report. Stereotact Funct Neurosurg. 1999; 72(Suppl 1):132–139. PMID: 10681701.
Article5. Loeffler JS, Rossitch E Jr, Siddon R, Moore MR, Rockoff MA, Alexander E 3rd. Role of stereotactic radiosurgery with a linear accelerator in treatment of intracranial arteriovenous malformations and tumors in children. Pediatrics. 1990; 5. 85(5):774–782. PMID: 2184409.
Article6. Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH, et al. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 1991; 10. 75(4):512–524. PMID: 1885968.
Article7. Marks MP, Delapaz RL, Fabrikant JI, Frankel KA, Phillips MH, Levy RP, et al. Intracranial vascular malformations: imaging of charged-particle radiosurgery. Part II. Complications. Radiology. 1988; 8. 168(2):457–462. PMID: 3293113.
Article8. Pollock BE, Gorman DA, Brown PD. Radiosurgery for arteriovenous malformations of the basal ganglia, thalamus, and brainstem. J Neurosurg. 2004; 2. 100(2):210–214. PMID: 15086226.
Article9. Potts MB, Young WL, Lawton MT. UCSF Brain AVM Study Project. Deep arteriovenous malformations in the Basal Ganglia, thalamus, and insula: microsurgical management, techniques, and results. Neurosurgery. 2013; 9. 73(3):417–429. PMID: 23728451.10. Uozumi Y, Sumitomo M, Maruwaka M, Araki Y, Izumi T, Miyachi S, et al. Moyamoya syndrome associated with gamma knife surgery for cerebral arteriovenous malformation: case report. Neurol Med Chir (Tokyo). 2012; 52(5):343–345. PMID: 22688073.11. Yamamoto M, Ide M, Jimbo M, Ono Y. Middle cerebral artery stenosis caused by relatively low-dose irradiation with stereotactic radiosurgery for cerebral arteriovenous malformations: case report. Neurosurgery. 1997; 8. 41(2):474–477. PMID: 9257317.
Article12. Yamamoto M, Jimbo M, Hara M, Saito I, Mori K. Gamma knife radiosurgery for arteriovenous malformations: long-term follow-up results focusing on complications occurring more than 5 years after irradiation. Neurosurgery. 1996; 5. 38(5):906–914. PMID: 8727815.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiosurgery for Cerebrovascular Disease
- Recurrence of pediatric cerebral arteriovenous malformation after obliteration by radiosurgery: a case report
- Gamma Knife Radiosurgery for Pediatric Arteriovenous Malformations
- A Potential Risk of Radiation-Induced Cavernous Malformations Following Adjuvant Gamma Knife Radiosurgery for Mesial Temporal Lobe Epilepsy
- Cyst Formation after Gamma Knife Radiosurgery for Cerebral Arteriovenous Malformation