J Korean Assoc Oral Maxillofac Surg.
2013 Dec;39(6):289-291. 10.5125/jkaoms.2013.39.6.289.
Wisdom teeth extraction in a patient with moyamoya disease
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Faculty of Medicine, Fukuoka University, Fukuoka, Japan. myamyu43729@yahoo.co.jp
- KMID: 1960979
- DOI: http://doi.org/10.5125/jkaoms.2013.39.6.289
Abstract
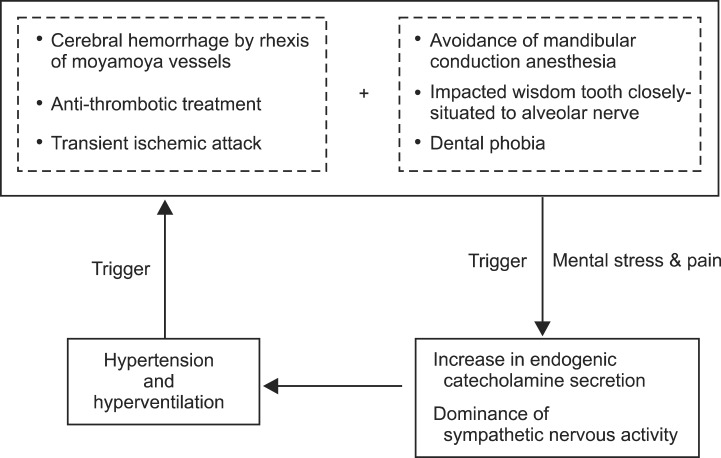
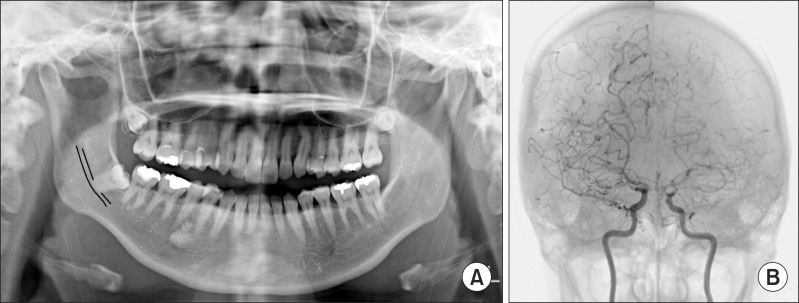
- Moyamoya disease is a rare neurovascular disorder that involves constriction of certain arteries in the brain. In patients with moyamoya disease, it is very important to prevent cerebral ischemic attacks and intracerebral bleeding caused by fluctuating blood pressure and increased respiration. A 40-year-old woman with moyamoya disease was scheduled for extraction of her right upper and lower impacted wisdom teeth. Her lower impacted wisdom tooth was situated close to the inferior alveolar nerve. We decided to continue her oral antiplatelet therapy and planned intravenous sedation with analgesic agents administered approximately five minutes prior to extraction of the root of the mandibular wisdom tooth. Oral analgesic medications were regularly administered postoperatively to alleviate pain and anxiety. During the perioperative period, no cerebrovascular event occurred, and the wisdom teeth were successfully extracted as per the planned procedure. It is thought that the perioperative risks of wisdom tooth extraction in patients with moyamoya disease can be minimized with the use of our protocols.
MeSH Terms
Figure
Reference
-
1. Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009; 360:1226–1237. PMID: 19297575.2. Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, Aoki R, et al. Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey. Clin Neurol Neurosurg. 1997; 99(Suppl 2):S1–S5. PMID: 9409395.
Article3. Iwama T, Hashimoto N, Yonekawa Y. The relevance of hemodynamic factors to perioperative ischemic complications in childhood moyamoya disease. Neurosurgery. 1996; 38:1120–1125. PMID: 8727141.
Article4. Kawaguchi T, Fujita S, Hosoda K, Shose Y, Hamano S, Iwakura M, et al. Multiple burr-hole operation for adult moyamoya disease. J Neurosurg. 1996; 84:468–476. PMID: 8609560.
Article5. Masaoka Y, Onaka Y, Shimizu Y, Sakurai S, Homma I. State anxiety dependent on perspiration during mental stress and deep inspiration. J Physiol Sci. 2007; 57:121–126. PMID: 17389060.
Article6. Homma S. The effects of stress in response to mirror drawing test trials on the electrogastrogram, heart rate and respiratory rate of human subjects. J Smooth Muscle Res. 2005; 41:221–233. PMID: 16258235.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications of impacted third molar extraction: retrospective study
- Kissing molars class III detected at a young age
- Target Controlled Conscious Sedation with Propofol and Remifentanil for the Extraction of Impacted Wisdom Teeth
- Neuroimaging Diagnosis and Treatment of Moyamoya Disease
- Moyamoya-like Disease Associated with Intracranial Aneurysm