J Korean Neurosurg Soc.
2014 Aug;56(2):162-165. 10.3340/jkns.2014.56.2.162.
Idiopathic Hypertrophic Spinal Pachymeningitis with an Osteolytic Lesion
- Affiliations
-
- 1Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. w.eoh@samsung.com
- KMID: 1956522
- DOI: http://doi.org/10.3340/jkns.2014.56.2.162
Abstract
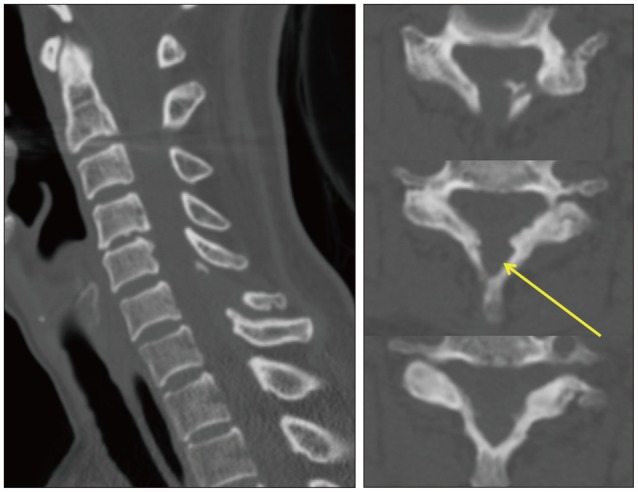
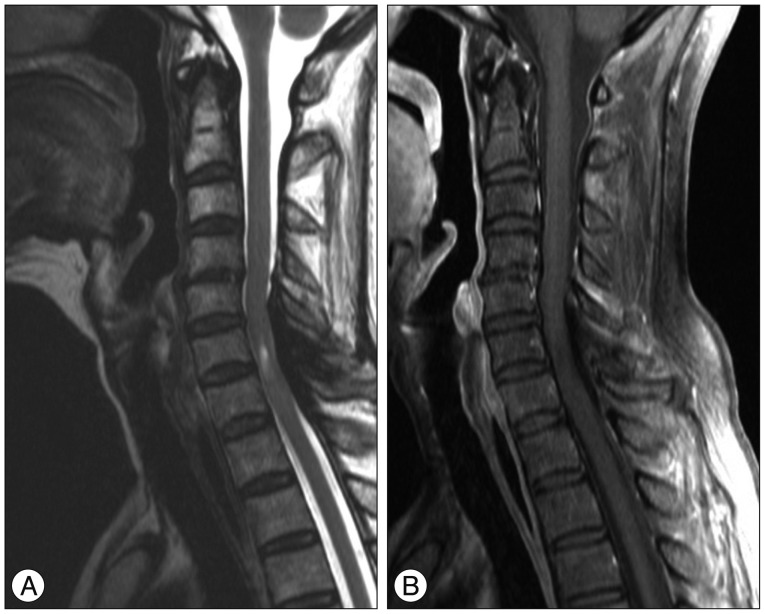
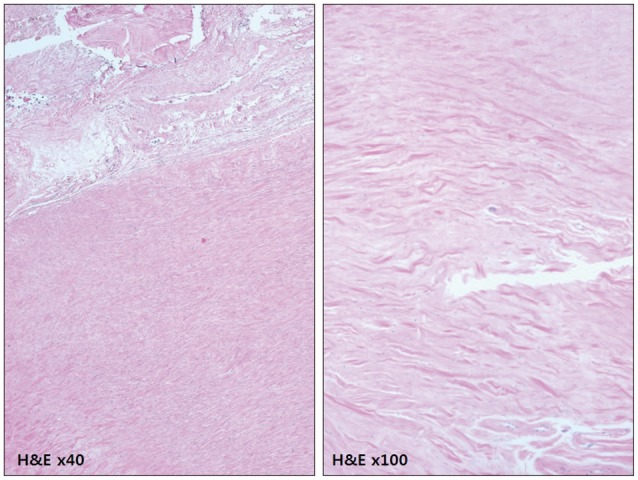
- Idiopathic hypertrophic spinal pachymeningitis (IHSP) is a chronic, progressive, inflammatory disorder characterized by marked fibrosis of the spinal dura mater with unknown etiology. According to the location of the lesion, it might induce neurologic deficits by compression of spinal cord and nerve root. A 58-year old female with a 3-year history of progressive weakness in both lower extremities was referred to our institute. Spinal computed tomography (CT) scan showed an osteolytic lesion involving base of the C6 spinous process with adjacent epidural mass. Magnetic resonance imaging (MRI) revealed an epidural mass involving dorsal aspect of cervical spinal canal from C5 to C7 level, with low signal intensity on T1 and T2 weighted images and non-enhancement on T1 weighted-enhanced images. We decided to undertake surgical exploration. At the operation field, there was yellow colored, thickened fibrous tissue over the dura mater. The lesion was removed totally, and decompression of spinal cord was achieved. Symptoms improved partially after the operation. Histopathologically, fibrotic pachymeninges with scanty inflammatory cells was revealed, which was compatible with diagnosis of idiopathic hypertrophic pachymeningitis. Six months after operation, motor power grade of both lower extremities was normal on physical examination. However, the patient still complained of mild weakness in the right lower extremity. Although the nature of IHSP is generally indolent, decompressive surgery should be considered for the patient with definite or progressive neurologic symptoms in order to prevent further deterioration. In addition, IHSP can present as an osteolytic lesion. Differential diagnosis with neoplastic disease, including giant cell tumor, is important.
Keyword
MeSH Terms
Figure
Reference
-
1. Adler JR, Sheridan W, Kosek J, Linder S. Pachymeningitis associated with a pulmonary nodule. Neurosurgery. 1991; 29:283–287. PMID: 1886671.
Article2. Agdal N, Hagdrup HK, Wantzin GL. Pachymeningitis cervicalis hypertrophica syphilitica. Acta Derm Venereol. 1980; 60:184–186. PMID: 6155037.3. Astrom KE, Lidholm SO. Extensive intracranial lesions in a case of orbital non-specific granuloma combined with polyarteritis nodosa. J Clin Pathol. 1963; 16:137–143. PMID: 13965307.
Article4. Bucy PC, Freeman LW. Hypertrophic spinal pachymeningitis with special reference to appropriate surgical treatment. J Neurosurg. 1952; 9:564–578. PMID: 13000476.
Article5. Dumont AS, Clark AW, Sevick RJ, Myles ST. Idiopathic hypertrophic pachymeningitis : a report of two patients and review of the literature. Can J Neurol Sci. 2000; 27:333–340. PMID: 11097527.
Article6. Friedman D, Flanders A, Tartaglino L. Contrast-enhanced MR imaging of idiopathic hypertrophic craniospinal pachymeningitis. AJR Am J Roentgenol. 1993; 160:900–901. PMID: 8456697.
Article7. Guidetti B, La Torre E. Hypertrophic spinal pachymeningitis. J Neurosurg. 1967; 26:496–503. PMID: 6025324.
Article8. Ito Z, Osawa Y, Matsuyama Y, Aoki T, Harada A, Ishiguro N. Recurrence of hypertrophic spinal pachymeningitis. Report of two cases and review of the literature. J Neurosurg Spine. 2006; 4:509–513. PMID: 16776365.9. Kao KP, Huang CI, Shan DE, Ho JT, Chang T, Chu FL. Non-obstructive idiopathic pachymeningitis cervicalis hypertrophica. J Neurol Neurosurg Psychiatry. 1986; 49:1441–1444. PMID: 3806122.
Article10. Kawano Y, Kira J. Chronic hypertrophic cranial pachymeningitis associated with HTLV-I infection. J Neurol Neurosurg Psychiatry. 1995; 59:435–437. PMID: 7561926.
Article11. Khadilkar SV, Menezes K, Parekh HN, Ursekar M, Bhagwati SN. Idiopathic hypertrophic cervical pachymeningitis : a case report with 5 year follow up. J Assoc Physicians India. 2003; 51:391–393. PMID: 12723656.12. Kim JH, Chin DK. Idiopathic hypertrophic spinal pachymeningitis : report of two cases and review of the literature. J Korean Neurosurg Soc. 2011; 50:392–395. PMID: 22200026.
Article13. Kupersmith MJ, Martin V, Heller G, Shah A, Mitnick HJ. Idiopathic hypertrophic pachymeningitis. Neurology. 2004; 62:686–694. PMID: 15007115.
Article14. Lee YC, Chueng YC, Hsu SW, Lui CC. Idiopathic hypertrophic cranial pachymeningitis : case report with 7 years of imaging follow-up. AJNR Am J Neuroradiol. 2003; 24:119–123. PMID: 12533339.15. Levine MR, Kaye L, Mair S, Bates J. Multifocal fibrosclerosis. Report of a case of bilateral idiopathic sclerosing pseudotumor and retroperitoneal fibrosis. Arch Ophthalmol. 1993; 111:841–843. PMID: 8512488.16. Martin N, Masson C, Henin D, Mompoint D, Marsault C, Nahum H. Hypertrophic cranial pachymeningitis : assessment with CT and MR imaging. AJNR Am J Neuroradiol. 1989; 10:477–484. PMID: 2501979.17. Mikawa Y, Watanabe R, Hino Y, Hirano K. Hypertrophic spinal pachymeningitis. Spine (Phila Pa 1976). 1994; 19:620–625. PMID: 8184360.
Article18. Moore AP, Rolfe EB, Jones EL. Pachymeningitis cranialis hypertrophica. J Neurol Neurosurg Psychiatry. 1985; 48:942–944. PMID: 4045489.
Article19. Naffziger HC, Stern WE. Chronic pachymeningitis; report of a case and review of the literature. Arch Neurol Psychiatry. 1949; 62:383–411.20. Nishino H, Rubino FA, Parisi JE. The spectrum of neurologic involvement in Wegener's granulomatosis. Neurology. 1993; 43:1334–1337. PMID: 8327134.
Article21. Nishizaki T, Iwamoto F, Uesugi S, Akimura T, Yamashita K, Ito H. Idiopathic cranial pachymeningoencephalitis focally affecting the parietal dura mater and adjacent brain parenchyma : case report. Neurosurgery. 1997; 40:840–843. discussion 843. PMID: 9092860.
Article22. Noble SC, Chandler WF, Lloyd RV. Intracranial extension of orbital pseudotumor : a case report. Neurosurgery. 1986; 18:798–801. PMID: 3736811.23. Pai S, Welsh CT, Patel S, Rumboldt Z. Idiopathic hypertrophic spinal pachymeningitis : report of two cases with typical MR imaging findings. AJNR Am J Neuroradiol. 2007; 28:590–592. PMID: 17353343.24. Park SH, Whang CJ, Sohn M, Oh YC, Lee CH, Whang YJ. Idiopathic hypertrophic spinal pachymeningitis : a case report. J Korean Med Sci. 2001; 16:683–688. PMID: 11641545.
Article25. Riku S, Kato S. Idiopathic hypertrophic pachymeningitis. Neuropathology. 2003; 23:335–344. PMID: 14719551.
Article26. Rosenfeld JV, Kaye AH, Davis S, Gonzales M. Pachymeningitis cervicalis hypertrophica. Case report. J Neurosurg. 1987; 66:137–139. PMID: 3783247.27. Schiess RJ, Coscia MF, McClellan GA. Petriellidium boydii pachymeningitis treated with miconazole and ketoconazole. Neurosurgery. 1984; 14:220–224. PMID: 6324020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rapid Recurrence of Spinal Idiopathic Hypertrophic Pachymeningitis: A Case Report
- Idiopathic Hypertrophic Pachymeningitis in the Craniocervical Junction
- A case of idiopathic hypertrophic pachymeningitis presented with seizures
- Idiopathic Hypertrophic Spinal Pachymeningitis: A Case Report
- Idiopathic Hypertrophic Cranial Pachymeningitis: Case Report