Prog Med Phys.
2014 Mar;25(1):37-45. 10.14316/pmp.2014.25.1.37.
Study of Scatter Influence of kV-Conebeam CT Based Calculation for Pelvic Radiotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. bcho@amc.seoul.kr
- 2Department of Biomedical Engineering, University of Biomedical Science and Engineering, Seoul, Korea.
- KMID: 1910557
- DOI: http://doi.org/10.14316/pmp.2014.25.1.37
Abstract
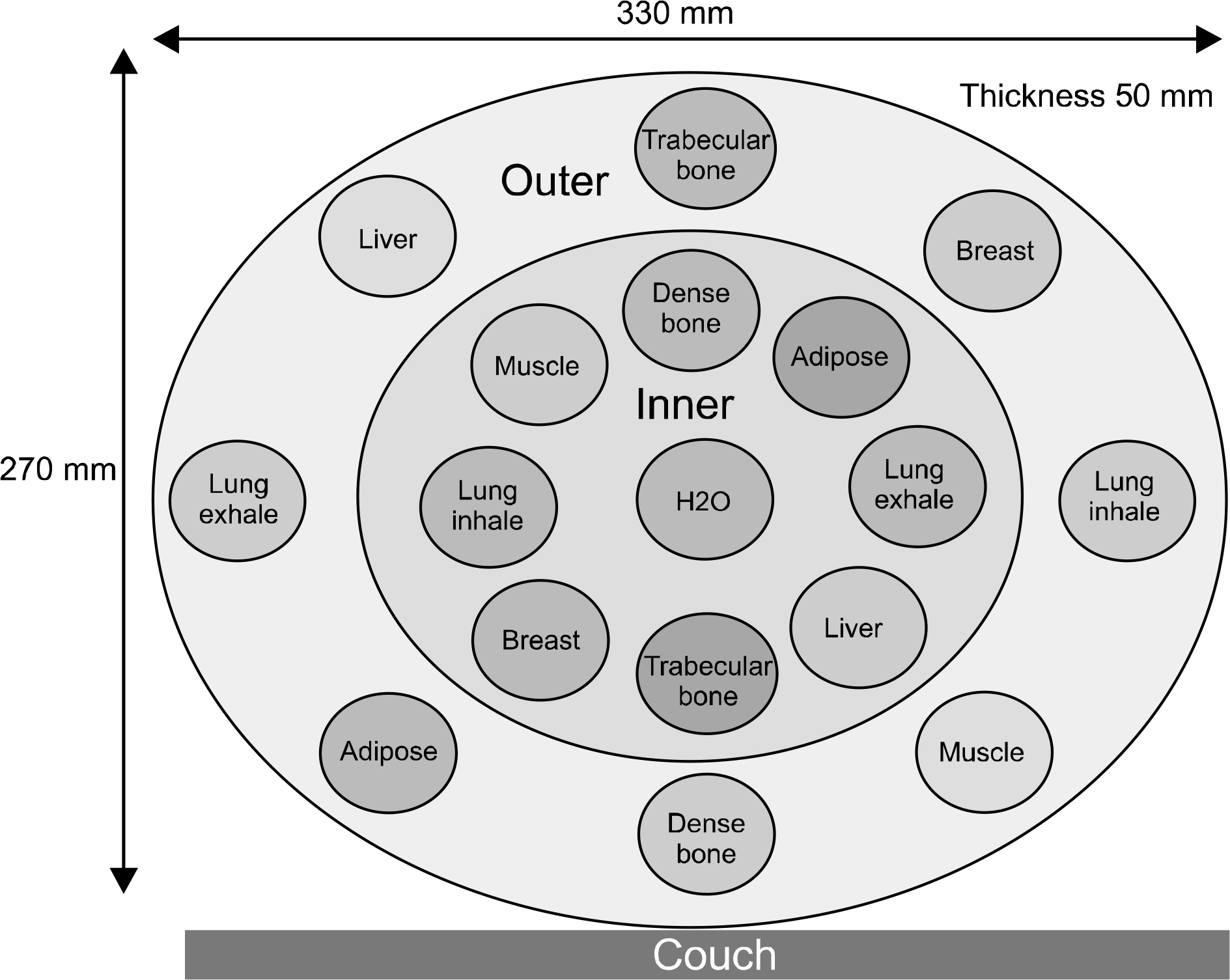
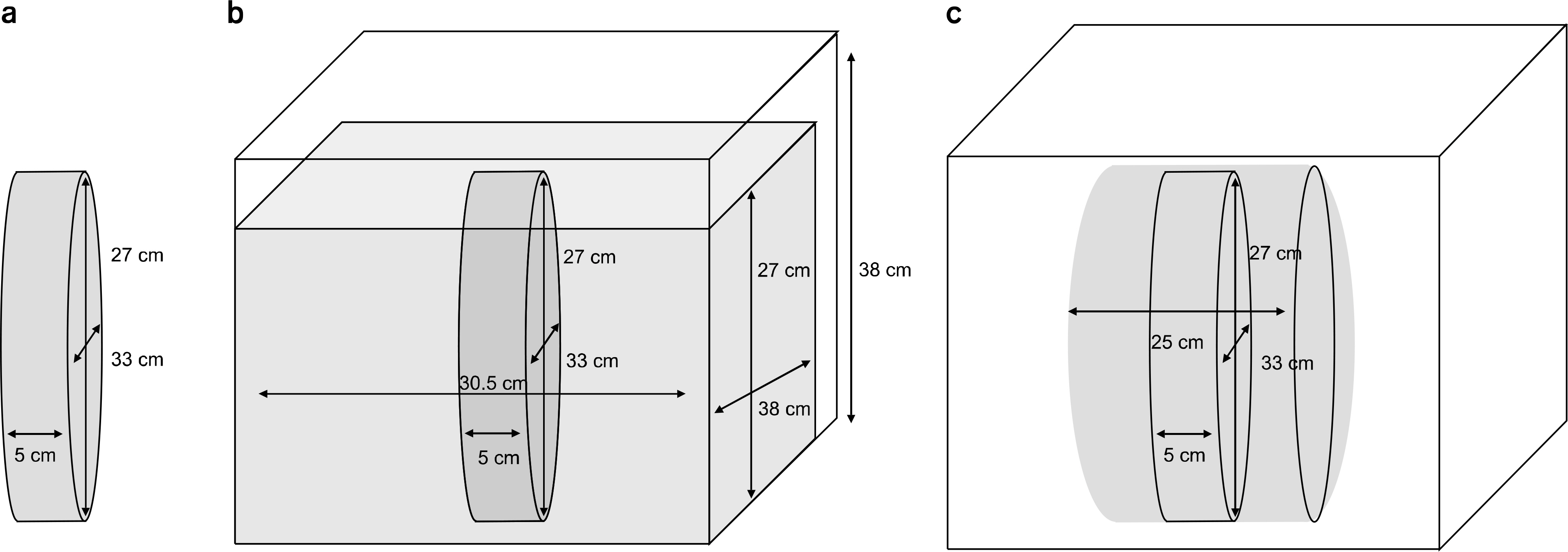
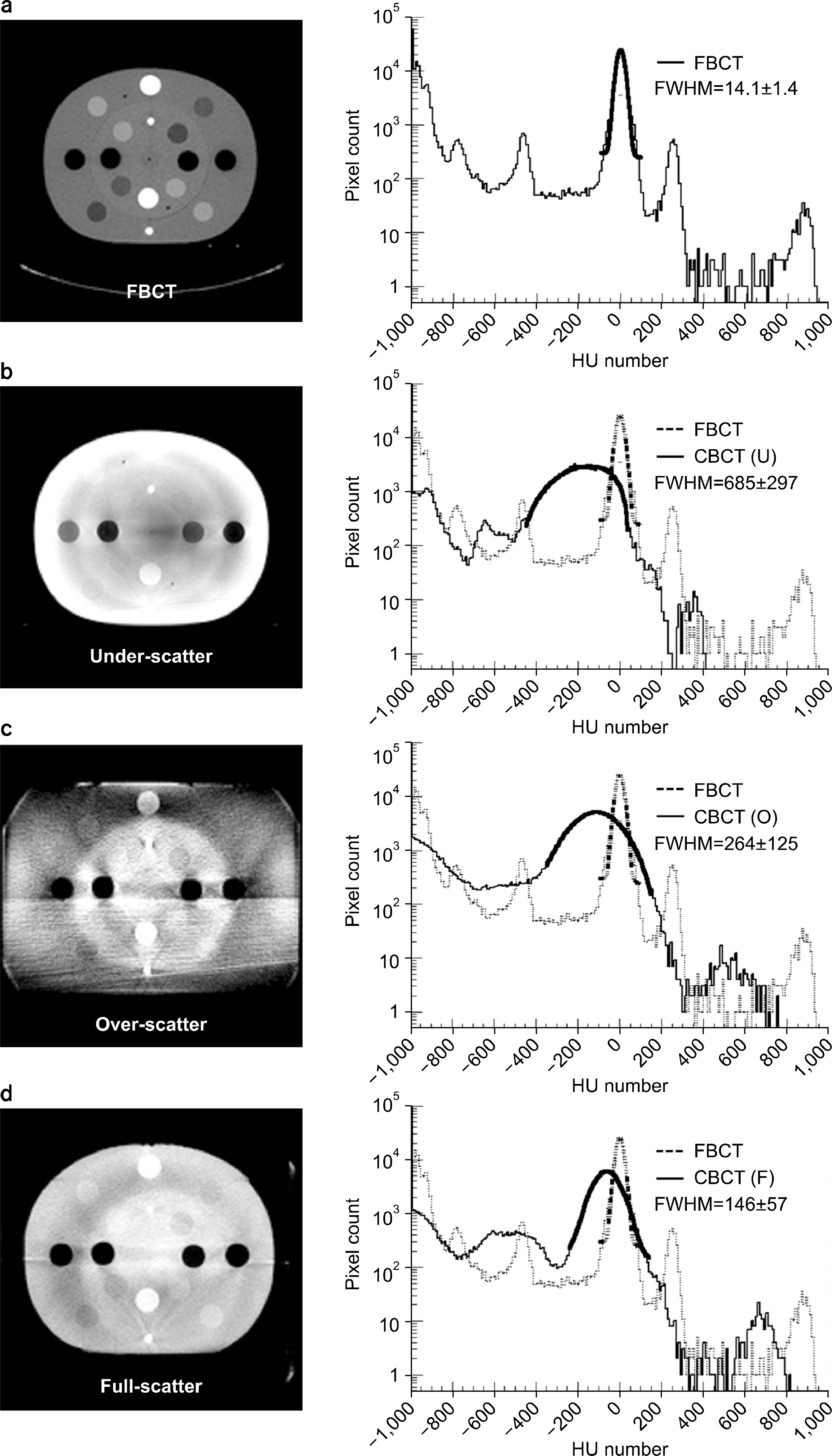
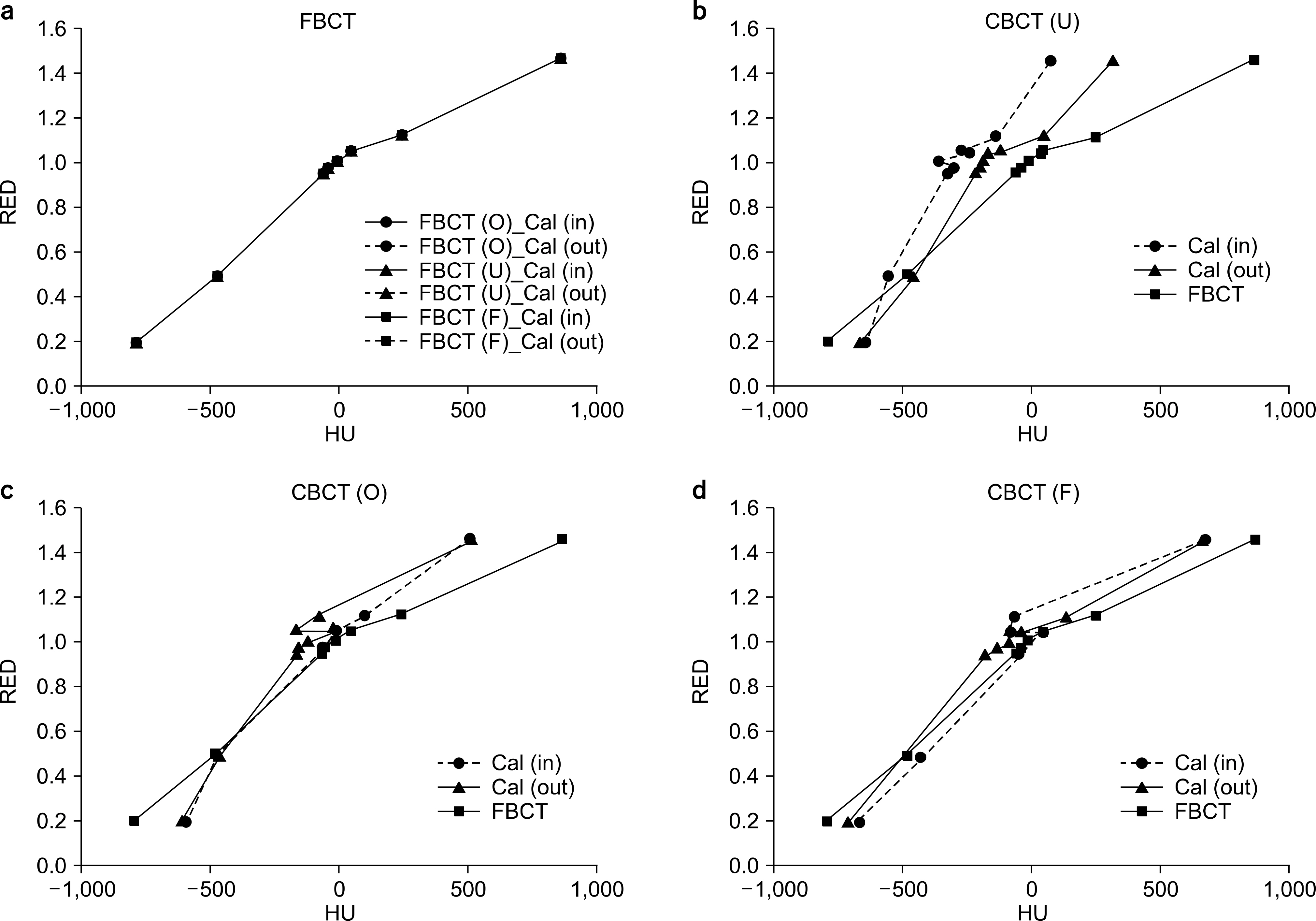
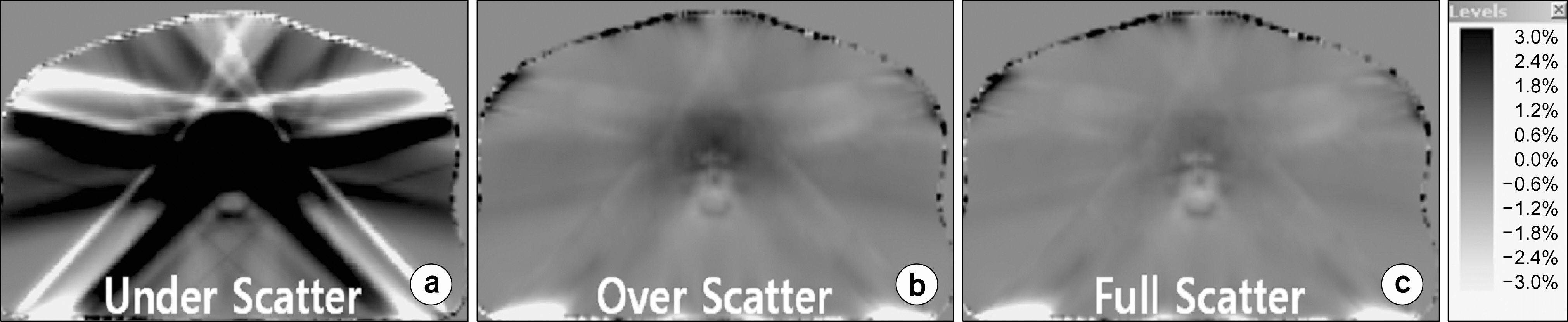
- The accuracy and uniformity of CT numbers are the main causes of radiation dose calculation error. Especially, for the dose calculation based on kV-Cone Beam Computed Tomography (CBCT) image, the scatter affecting the CT number is known to be quite different by the object sizes, densities, exposure conditions, and so on. In this study, the scatter impact on the CBCT based dose calculation was evaluated to provide the optimal condition minimizing the error. The CBCT images was acquired under three scatter conditions ("Under-scatter", "Over-scatter", and "Full-scatter") by adjusting amount of scatter materials around a electron density phantom (CIRS062, Tissue Simulation Technology, Norfolk, VA, USA). The CT number uniformities of CBCT images for water-equivalent materials of the phantom were assessed, and the location dependency, either "inner" or "outer" parts of the phantom, was also evaluated. The electron density correction curves were derived from CBCT images of the electron density phantom in each scatter condition. The electron density correction curves were applied to calculate the CBCT based doses, which were compared with the dose based on Fan Beam Computed Tomography (FBCT). Also, 5 prostate IMRT cases were enrolled to assess the accuracy of dose based on CBCT images using gamma index analysis and relative dose differences. As the CT number histogram of phantom CBCT images for water equivalent materials was fitted with a gaussian function, the FHWM (146 HU) for "Full-scatter" condition was the smallest among the FHWM for the three conditions (685 HU for "under scatter" and 264 HU for "over scatter"). Also, the variance of CT numbers was the smallest for the same ingredients located in the center and periphery of the phantom in the "Full-scatter" condition. The dose distributions calculated with FBCT and CBCT images compared in a gamma index evaluation of 1%/3 mm criteria and in the dose difference. With the electron density correction acquired in the same scatter condition, the CBCT based dose calculations tended to be the most accurate. In 5 prostate cases in which the mean equivalent diameter was 27.2 cm, the averaged gamma pass rate was 98% and the dose difference confirmed to be less than 2% (average 0.2%, ranged from -1.3% to 1.6%) with the electron density correction of the "Full-scatter" condition. The accuracy of CBCT based dose calculation could be confirmed that closely related to the CT number uniformity and to the similarity of the scatter conditions for the electron density correction curve and CBCT image. In pelvic cases, the most accurate dose calculation was achievable in the application of the electron density curves of the "Full-scatter" condition.
MeSH Terms
Figure
Reference
-
1. Xing L, et al. Overview of image-guided radiation therapy. Med Dosim. 31(2):91–112. 2006.
Article2. Hector CL, Webb S, Evans PM, et al. The dosimetric consequences of inter-fractional patient movement on conventional and intensity-modulated breast radiotherapy treatments. Radiother Oncol. 54(1):57–64. 2000.
Article3. Coolens C, et al. The susceptibility of IMRT dose distributions to intrafraction organ motion: an investigation into smoothing filters derived from four dimensional computed tomography data. Med Phys. 33(8):2809–2818. 2006.
Article4. Hugo GD, Agazaryan N, Solberg TD, et al. The effects of tumor motion on planning and delivery of respiratory-gated IMRT. Med Phys. 30(6):1052–1066. 2003.
Article5. Yoo S, Yin FF, et al. Dosimetric feasibility of cone-beam CT-based treatment planning compared to CT-based treatment planning. Int J Radiat Oncol Biol Phys. 66(5):1553–61. 2006.
Article6. Ding GX, et al. A study on adaptive IMRT treatment planning using kV cone-beam CT. Radiother Oncol. 85(1):116–25. 2007.
Article7. Siewerdsen JH, Jaffray DA, et al. Cone-beam computed tomography with a flat-panel imager: magnitude and effects of x-ray scatter. Medical physics. 28(2):220–231. 2001.
Article8. Lee L, Le QT, Xing L, et al. Retrospective IMRT dose reconstruction based on cone-beam CT and MLC log-file. Int J Radiat Oncol Biol Phys. 70(2):634–344. 2008.
Article9. Guan H, Dong H, et al. Dose calculation accuracy using cone-beam CT (CBCT) for pelvic adaptive radiotherapy. Phys Med Biol. 54(20):6239–6250. 2009.
Article10. Yang Y, et al. Evaluation of on-board kV cone beam CT (CBCT)-based dose calculation. Phys Med Biol. 52(3):685–705. 2007.
Article11. Rong Y, et al. Dose calculation on kV cone beam CT images: an investigation of the Hu-density conversion stability and dose accuracy using the site-specific calibration. Med Dosim. 35(3):195–207. 2010.
Article12. Endoa Masahiro, et al. Effect of scattered radiation on image noise in cone beam CT. Med Phys. 28:469. 2001.13. Calvo Ortega JF, et al. A dosimetric evaluation of the Eclipse AAA algorithm and Millennium 120 MLC for cranial intensity-modulated radiosurgery. Med Dosim. 2013.
Article14. Lu W, et al. Deformable registration of the planning image (kVCT) and the daily images (MVCT) for adaptive radiation therapy. Phys Med Biol. 51(17):4357–4374. 2006.
Article15. Matsinos E, et al. Current status of the CBCT project at Varian Medical Systems Proc. SPIE. 5745. 340–351. (2005).
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improvement of the Dose Calculation Accuracy Using MVCBCT Image Processing
- Feasibility of Improving the Accuracy of Dose Calculation Using Hybrid Computed Tomography Images: A Phantom Study
- An Experimental Method for the Scatter Correction of MV Images Using Scatter to Primary Ratios (SPRs)
- Measurement and Evaluation of Scatter Fractions for Digital Radiography with a Beam-Stop Array
- The Effect of the CT Number for Each CT on Dose Calculation