Ann Surg Treat Res.
2014 May;86(5):264-269. 10.4174/astr.2014.86.5.264.
Hiatal hernia in pediatric patients: laparoscopic versus open approaches
- Affiliations
-
- 1Division of Pediatric Surgery, Department of Surgery, Asan Medical Center, Seoul, Korea. kimdy@amc.seoul.kr
- KMID: 1889664
- DOI: http://doi.org/10.4174/astr.2014.86.5.264
Abstract
- PURPOSE
The aim of this study was to evaluate the surgical outcomes of laparoscopic approach for hiatal hernia (HH) in pediatric patients.
METHODS
This was a retrospective study of 33 patients younger than 18 years who underwent an operation for HH between January 1999 and December 2012.
RESULTS
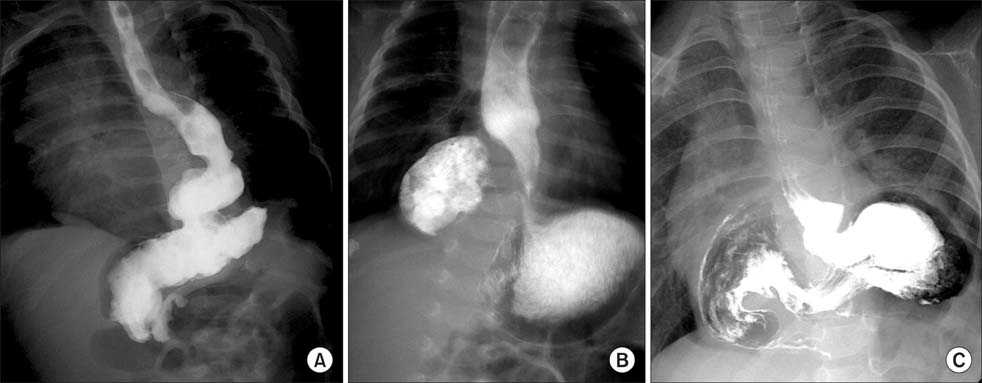
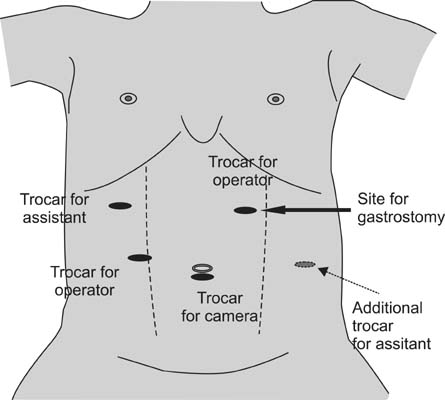
The HH symptoms were various and included regurgitation, vomiting, weight loss, cough, hoarseness, and cyanosis. Among the 33 patients, there were 25 sliding types, 1 paraesophageal type, and 7 mixed types. Open surgery (OS) and laparoscopic surgery (LS) were used in 16 and 17 patients, respectively. There were no statistically significant differences in sex, age, or body weight between the groups. The median operating time was longer in the LS group (150 minutes; range, 90-250 minutes vs. 125 minutes; range, 66-194 minutes; P = 0.028). Time to oral intake was shorter in the LS group than in the OS group (1 day; range, 1-3 days vs. 2 days; range, 1-7 days; P = 0.001) and time to full feeding was shorter in the LS group than in the OS group (6 days; range, 3-16 days vs. 10 days; range, 3-33 days; P = 0.048). There were no differences in length of hospital stay and complications between the two groups. There was no perioperative mortality or recurrence of HH.
CONCLUSION
A good surgical outcome for laparoscopic correction of HH was seen in pediatric patients.
MeSH Terms
Figure
Cited by 1 articles
-
The outcome of hiatal hernia repair and factors associated with surgical outcome in the pediatric population: a single-center experience
Sujin Gang, Hyunhee Kwon, Jueun Park, Dae Yeon Kim
Ann Surg Treat Res. 2023;105(6):396-403. doi: 10.4174/astr.2023.105.6.396.
Reference
-
1. Stylopoulos N, Rattner DW. The history of hiatal hernia surgery: from Bowditch to laparoscopy. Ann Surg. 2005; 241:185–193.2. Mitiek MO, Andrade RS. Giant hiatal hernia. Ann Thorac Surg. 2010; 89:S2168–S2173.3. Fullum TM, Oyetunji TA, Ortega G, Tran DD, Woods IM, Obayomi-Davies O, et al. Open versus laparoscopic hiatal hernia repair. JSLS. 2013; 17:23–29.4. Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967; 53:33–54.5. Lee JW, Kim HS, Ryu BY, Kim HK, Han SJ. Paraesophageal hernia with small bowel strangulation. J Korean Surg Soc. 2010; 78:195–198.6. Jang WN, Park IS, Park KW, Yoo SY, Lee J, Cho SH. A case of congenital paraesophageal hiatal hernia in infancy. Pediatr Gastroenterol Hepatol Nutr. 2012; 15:100–104.7. Hashemi M, Sillin LF, Peters JH. Current concepts in the management of paraesophageal hiatal hernia. J Clin Gastroenterol. 1999; 29:8–13.8. Weber C, Davis CS, Shankaran V, Fisichella PM. Hiatal hernias: a review of the pathophysiologic theories and implication for research. Surg Endosc. 2011; 25:3149–3153.9. Aly A, Munt J, Jamieson GG, Ludemann R, Devitt PG, Watson DI. Laparoscopic repair of large hiatal hernias. Br J Surg. 2005; 92:648–653.10. Yagi M, Nose K, Yamauchi K, Nogami T, Yoshida H, Okuyama H, et al. Laparoscopic intervention for intrathoracic stomach in infants. Surg Endosc. 2003; 17:1636–1639.11. van der Zee DC, Bax NM, Kramer WL, Mokhaberi B, Ure BM. Laparoscopic management of a paraesophageal hernia with intrathoracic stomach in infants. Eur J Pediatr Surg. 2001; 11:52–54.12. Bradley T, Stephenson J, Drugas G, Avansino JR. Laparoscopic management of neonatal paraesophageal hernia with intrathoracic gastric volvulus. J Pediatr Surg. 2010; 45:E21–E23.13. Esposito C, Montupet P, van Der Zee D, Settimi A, Paye-Jaouen A, Centonze A, et al. Long-term outcome of laparoscopic Nissen, Toupet, and Thal antireflux procedures for neurologically normal children with gastroesophageal reflux disease. Surg Endosc. 2006; 20:855–858.14. Esposito C, Montupet P, Reinberg O. Laparoscopic surgery for gastroesophageal reflux disease during the first year of life. J Pediatr Surg. 2001; 36:715–717.15. Fernando HC, Luketich JD, Christie NA, Ikramuddin S, Schauer PR. Outcomes of laparoscopic Toupet compared to laparoscopic Nissen fundoplication. Surg Endosc. 2002; 16:905–908.16. Kubiak R, Andrews J, Grant HW. Long-term outcome of laparoscopic nissen fundoplication compared with laparoscopic thal fundoplication in children: a prospective, randomized study. Ann Surg. 2011; 253:44–49.17. Kubiak R, Andrews J, Grant HW. Laparoscopic Nissen fundoplication versus Thal fundoplication in children: comparison of short-term outcomes. J Laparoendosc Adv Surg Tech A. 2010; 20:665–669.18. Ashcraft KW, Goodwin CD, Amoury RW, McGill CW, Holder TM. Thal fundoplication: a simple and safe operative treatment for gastroesophageal reflux. J Pediatr Surg. 1978; 13(6D):643–647.19. Li J, Rosenthal RJ, Roy M, Szomstein S, Sesto M. Experience of laparoscopic paraesophageal hernia repair at a single institution. Am J Surg. 2012; 204:60–65.20. Nason KS, Luketich JD, Witteman BP, Levy RM. The laparoscopic approach to paraesophageal hernia repair. J Gastrointest Surg. 2012; 16:417–426.21. Wassenaar EB, Mier F, Sinan H, Petersen RP, Martin AV, Pellegrini CA, et al. The safety of biologic mesh for laparoscopic repair of large, complicated hiatal hernia. Surg Endosc. 2012; 26:1390–1396.22. Furnée E, Hazebroek E. Mesh in laparoscopic large hiatal hernia repair: a systematic review of the literature. Surg Endosc. 2013; 27:3998–4008.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Sliding Hiatal Hernia associated with Bochdalek Hernia Repair
- Characteristics and recent therapeutic trends of pediatric inguinal hernia
- Two Cases of Bochdalek Hernia and One Case of Hiatal Hernia
- Congenital Hiatal Hernia Associated with Anemia
- The outcome of hiatal hernia repair and factors associated with surgical outcome in the pediatric population: a single-center experience