Ann Surg Treat Res.
2014 May;86(5):249-255. 10.4174/astr.2014.86.5.249.
Comparison of abdominal and perineal procedures for complete rectal prolapse: an analysis of 104 patients
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jckim@amc.seoul.kr
- 2Department of Surgery, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 1889662
- DOI: http://doi.org/10.4174/astr.2014.86.5.249
Abstract
- PURPOSE
Selecting the best surgical approach for treating complete rectal prolapse involves comparing the operative and functional outcomes of the procedures. The aims of this study were to evaluate and compare the operative and functional outcomes of abdominal and perineal surgical procedures for patients with complete rectal prolapse.
METHODS
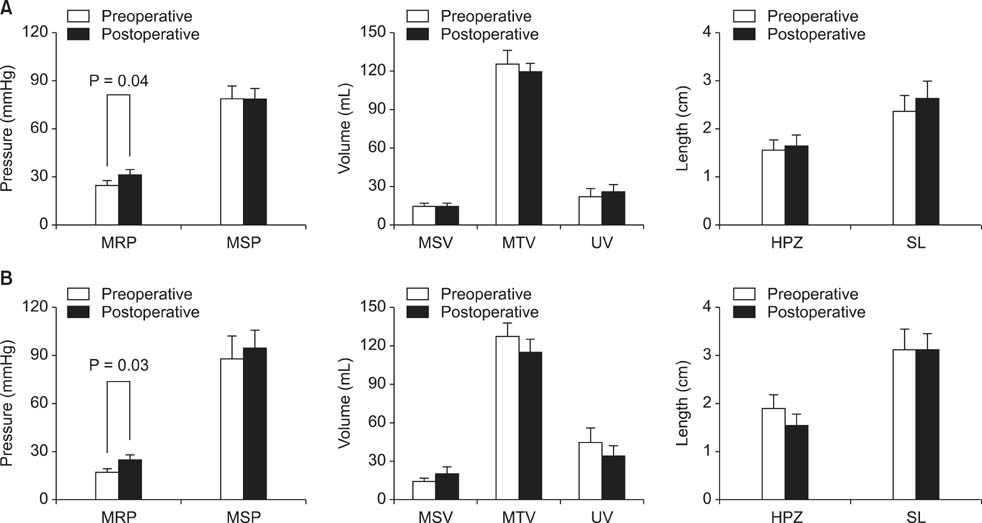
A retrospective study of patients with complete rectal prolapse who had operations at a tertiary referral hospital and a university hospital between March 1990 and May 2011 was conducted. Patients were classified according to the type of operation: abdominal procedure (AP) (n = 64) or perineal procedure (PP) (n = 40). The operative outcomes and functional results were assessed.
RESULTS
The AP group had the younger and more men than the PP group. The AP group had longer operation times than the PP group (165 minutes vs. 70 minutes; P = 0.001) and longer hospital stays (10 days vs. 7 days; P = 0.001), but a lower overall recurrence rate (6.3% vs. 15.0%; P = 0.14). The overall rate of the major complication was similar in the both groups (10.9% vs. 6.8%; P = 0.47). The patients in the AP group complained more frequently of constipation than of incontinence, conversely, in the PP group of incontinence than of constipation.
CONCLUSION
The two approaches for treating complete rectal prolapse did not differ with regard to postoperative morbidity, but the overall recurrence tended to occur frequently among patients in the PP group. Functional results after each surgical approach need to be considered for the selection of procedure.
Keyword
MeSH Terms
Figure
Reference
-
1. Riansuwan W, Hull TL, Bast J, Hammel JP, Church JM. Comparison of perineal operations with abdominal operations for full-thickness rectal prolapse. World J Surg. 2010; 34:1116–1122.2. Schultz I, Mellgren A, Dolk A, Johansson C, Holmstrom B. Long-term results and functional outcome after Ripstein rectopexy. Dis Colon Rectum. 2000; 43:35–43.3. Kim DS, Tsang CB, Wong WD, Lowry AC, Goldberg SM, Madoff RD. Complete rectal prolapse: evolution of management and results. Dis Colon Rectum. 1999; 42:460–466.4. Luukkonen P, Mikkonen U, Jarvinen H. Abdominal rectopexy with sigmoidectomy vs. rectopexy alone for rectal prolapse: a prospective, randomized study. Int J Colorectal Dis. 1992; 7:219–222.5. Finlay IG, Aitchison M. Perineal excision of the rectum for prolapse in the elderly. Br J Surg. 1991; 78:687–689.6. Brown AJ, Anderson JH, McKee RF, Finlay IG. Strategy for selection of type of operation for rectal prolapse based on clinical criteria. Dis Colon Rectum. 2004; 47:103–107.7. Fleming FJ, Kim MJ, Gunzler D, Messing S, Monson JR, Speranza JR. It's the procedure not the patient: the operative approach is independently associated with an increased risk of complications after rectal prolapse repair. Colorectal Dis. 2012; 14:362–368.8. McMahan JD, Ripstein CB. Rectal prolapse. An update on the rectal sling procedure. Am Surg. 1987; 53:37–40.9. Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996; 39:681–685.10. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993; 36:77–97.11. Gourgiotis S, Baratsis S. Rectal prolapse. Int J Colorectal Dis. 2007; 22:231–243.12. Yoon SG. Rectal prolapse: review according to the personal experience. J Korean Soc Coloproctol. 2011; 27:107–113.13. Yoon SG, Lee KR, Cho KA, Hwang DY, Kim KU, Kang YW, et al. Clinical and physiologic characteristics of rectal prolapse in males. J Korean Soc Coloproctol. 2000; 16:223–230.14. Madiba TE, Baig MK, Wexner SD. Surgical management of rectal prolapse. Arch Surg. 2005; 140:63–73.15. Kuijpers HC. Treatment of complete rectal prolapse: to narrow, to wrap, to suspend, to fix, to encircle, to plicate or to resect? World J Surg. 1992; 16:826–830.16. Yakut M, Kaymakcioglu N, Simsek A, Tan A, Sen D. Surgical treatment of rectal prolapse. A retrospective analysis of 94 cases. Int Surg. 1998; 83:53–55.17. Husa A, Sainio P, von Smitten K. Abdominal rectopexy and sigmoid resection (Frykman-Goldberg operation) for rectal prolapse. Acta Chir Scand. 1988; 154:221–224.18. Graf W, Karlbom U, Pahlman L, Nilsson S, Ejerblad S. Functional results after abdominal suture rectopexy for rectal prolapse or intussusception. Eur J Surg. 1996; 162:905–911.19. Delemarre JB, Gooszen HG, Kruyt RH, Soebhag R, Geesteranus AM. The effect of posterior rectopexy on fecal continence: a prospective study. Dis Colon Rectum. 1991; 34:311–316.20. Ashari LH, Lumley JW, Stevenson AR, Stitz RW. Laparoscopically-assisted resection rectopexy for rectal prolapse: ten years' experience. Dis Colon Rectum. 2005; 48:982–987.21. Ahmad M, Sileri P, Franceschilli L, Mercer-Jones M. The role of biologics in pelvic floor surgery. Colorectal Dis. 2012; 14:Suppl 3. 19–23.22. Glasgow SC, Birnbaum EH, Kodner IJ, Fleshman JW, Dietz DW. Preoperative anal manometry predicts continence after perineal proctectomy for rectal prolapse. Dis Colon Rectum. 2006; 49:1052–1058.23. Ris F, Colin JF, Chilcott M, Remue C, Jamart J, Kartheuser A. Altemeier's procedure for rectal prolapse: analysis of long-term outcome in 60 patients. Colorectal Dis. 2012; 14:1106–1111.24. Park HJ, So BJ, Jun KY. Comparative analysis of operative procedures in rectal prolapse between perineal and abdominal approach. J Korean Surg Soc. 1991; 40:354–359.25. Formijne Jonkers HA, Draaisma WA, Wexner SD, Broeders IA, Bemelman WA, Lindsey I, et al. Evaluation and surgical treatment of rectal prolapse: an international survey. Colorectal Dis. 2013; 15:115–119.26. D'Hoore A, Cadoni R, Penninckx F. Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg. 2004; 91:1500–1505.27. Wijffels N, Cunningham C, Dixon A, Greenslade G, Lindsey I. Laparoscopic ventral rectopexy for external rectal prolapse is safe and effective in the elderly. Does this make perineal procedures obsolete? Colorectal Dis. 2011; 13:561–566.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complete Rectal Prolapse Combined with Rectal Cancer: A Case Report
- Rectal Prolapse: Review According to the Personal Experience
- Comparative analysis of operative procedures in rectal prolapse between perineal and abdominal approach
- Comparison of abdominal and perineal approach for recurrent rectal prolapse
- Surgical Treatment of Rectal Prolapse: A 10-Year Experience at a Single Institution