J Korean Soc Transplant.
2013 Dec;27(4):153-159. 10.4285/jkstn.2013.27.4.153.
Histopathological Features of Late Liver Allograft Dysfunction
- Affiliations
-
- 1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. d890075@gmail.com
- KMID: 1841123
- DOI: http://doi.org/10.4285/jkstn.2013.27.4.153
Abstract
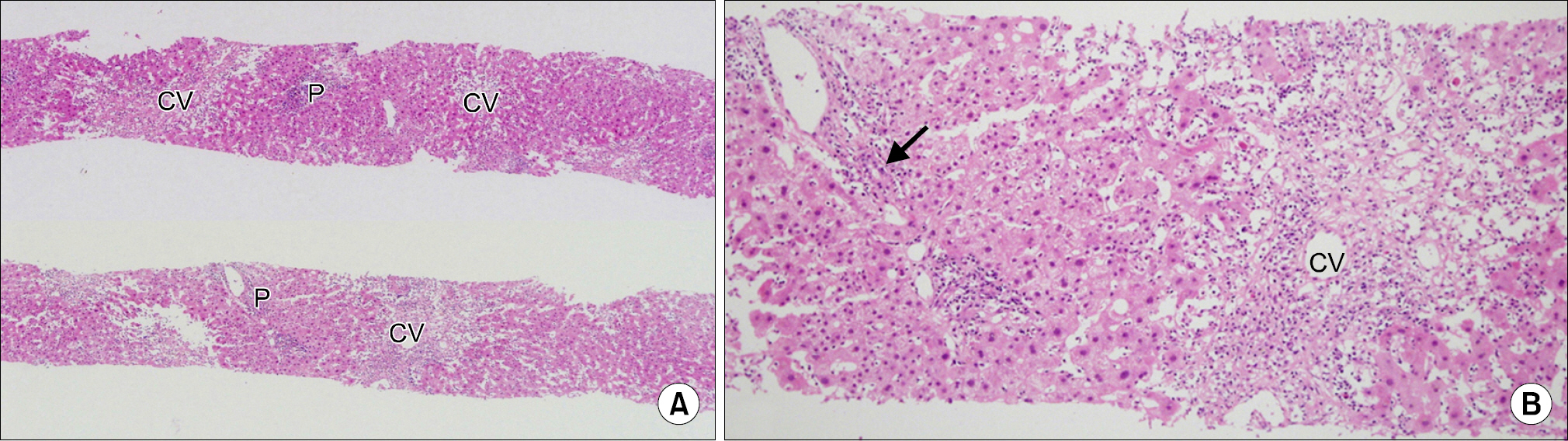
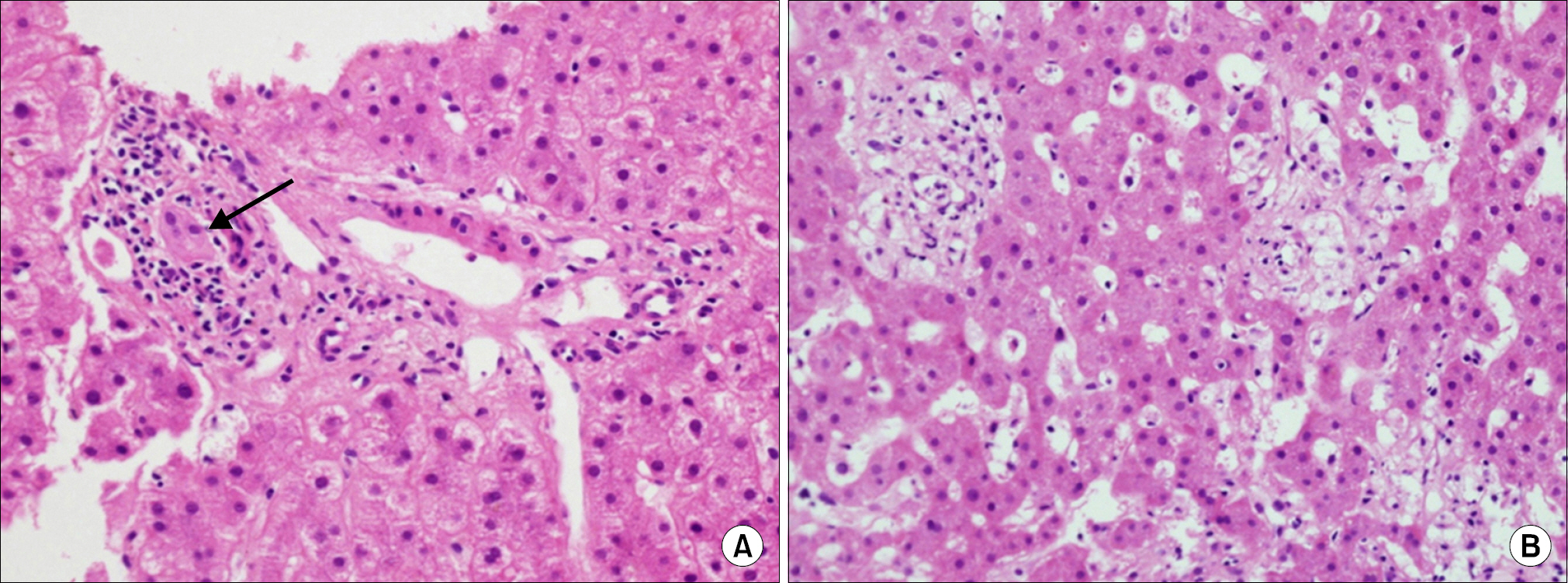
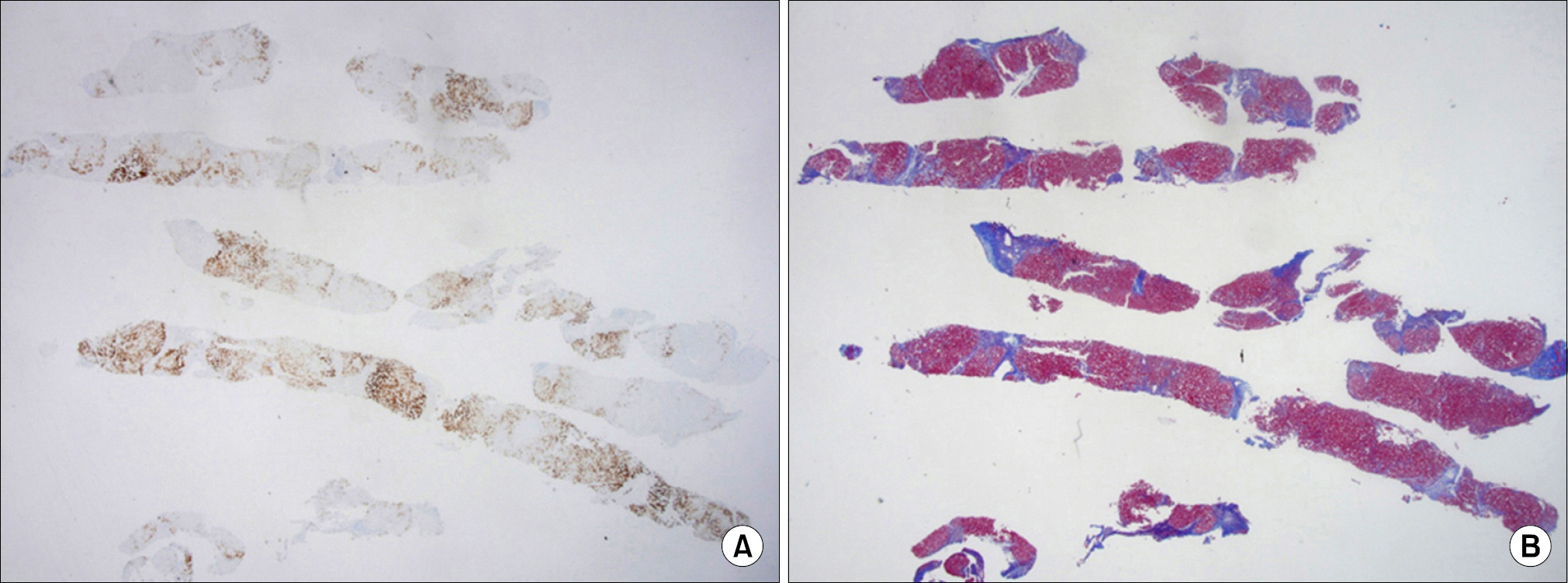
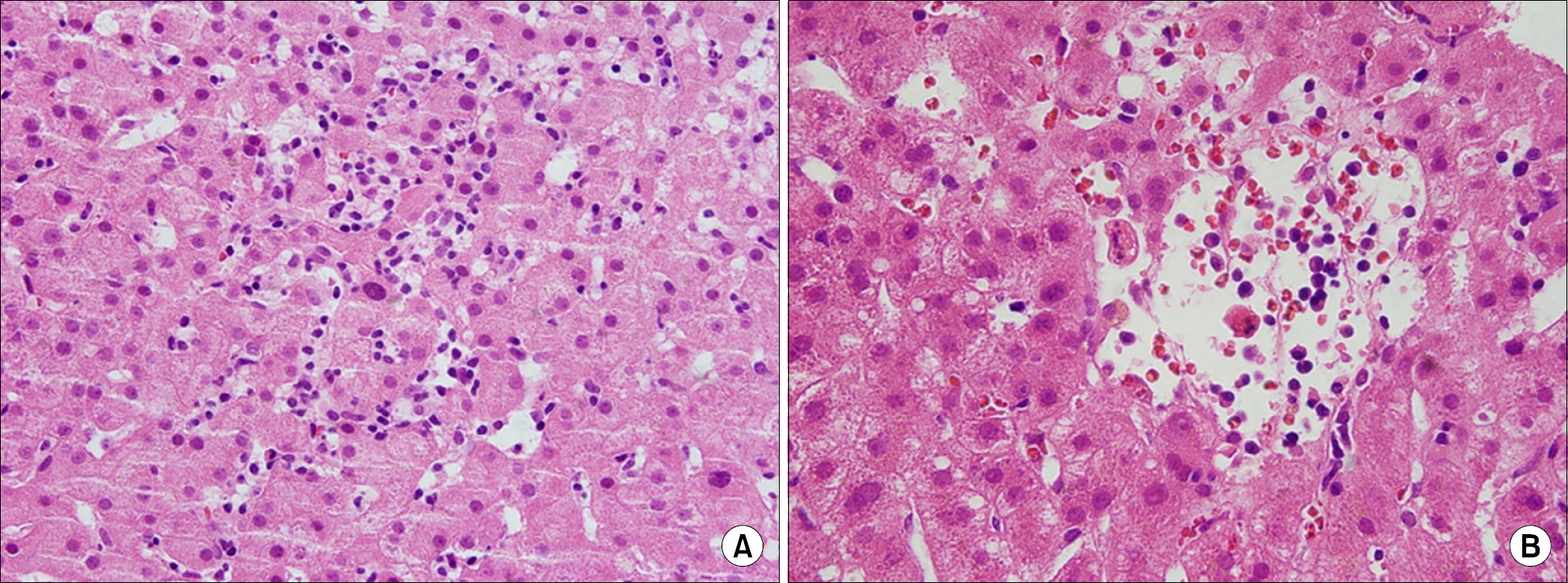
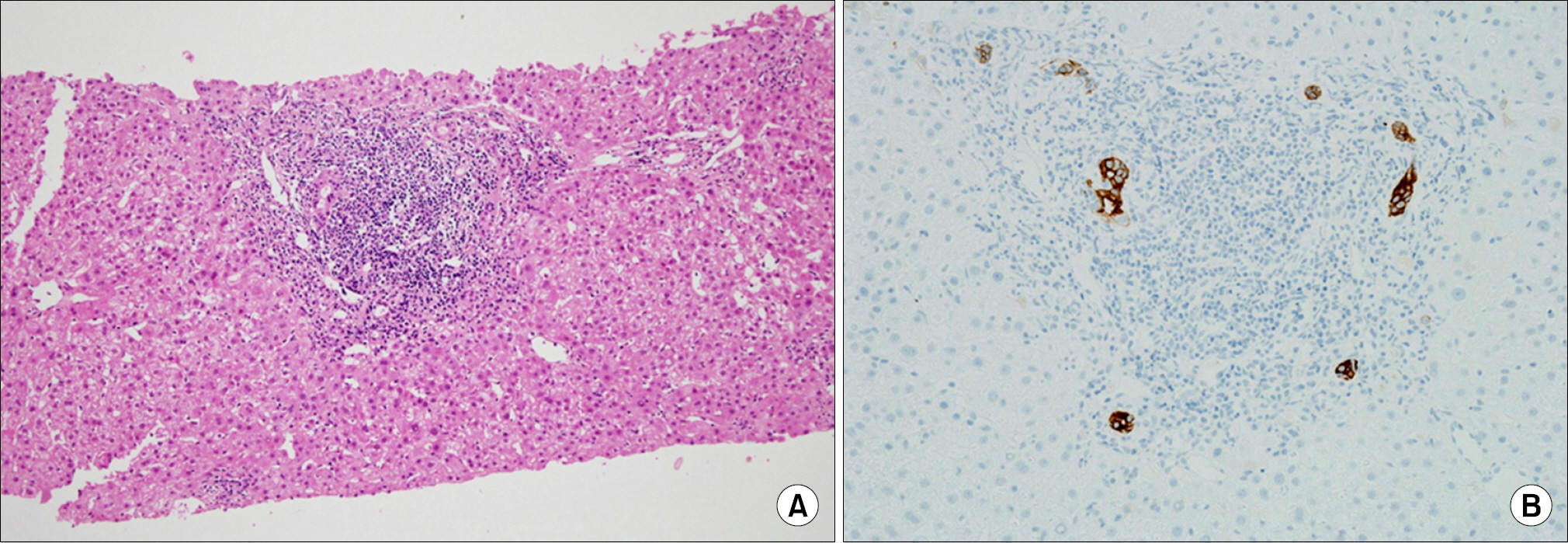
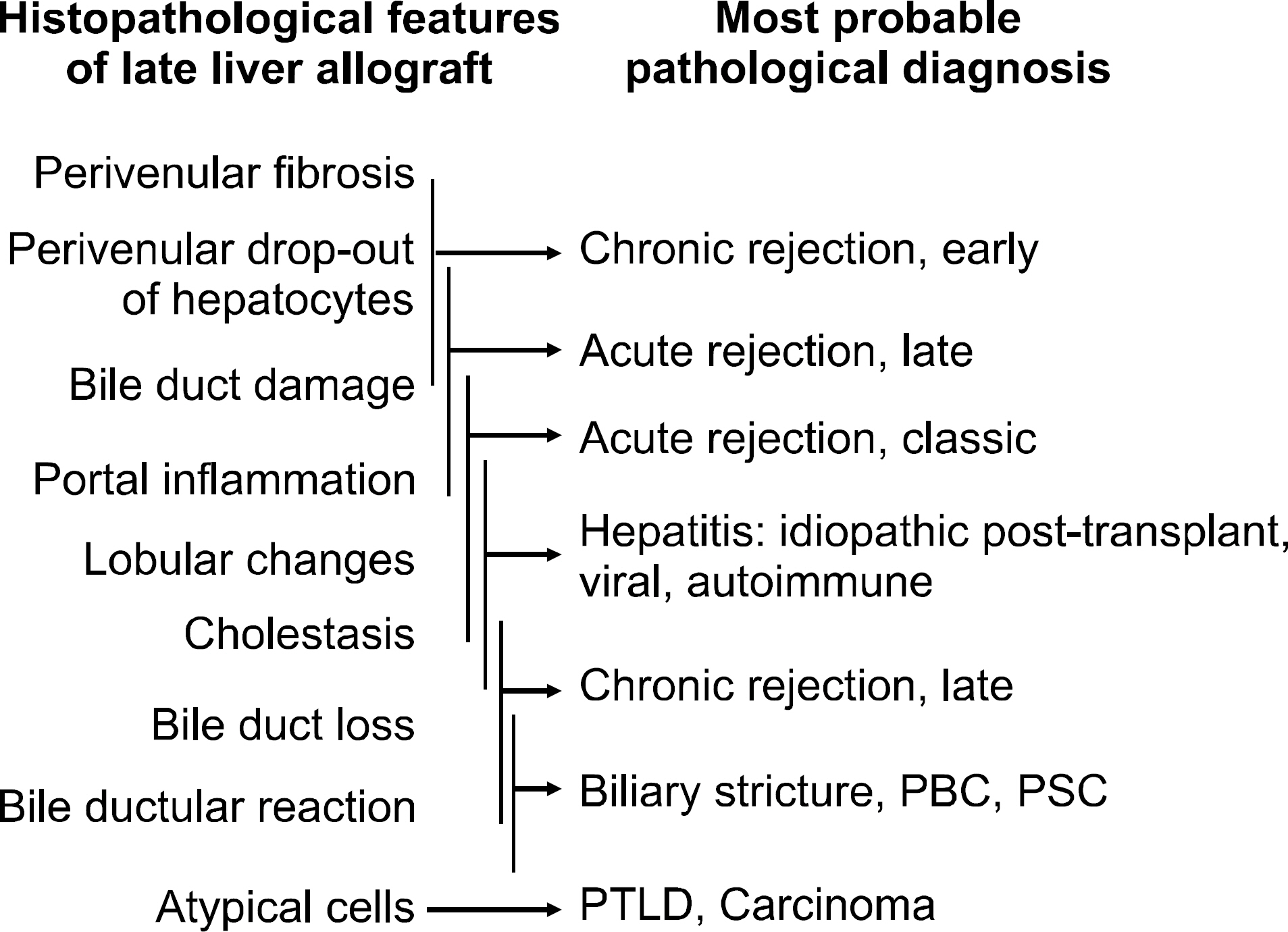
- Interpretation of late allograft biopsies can be challenging because of overlapping clinicopathological features, regional difference of underlying liver diseases for liver transplantation, and continuous changing of preoperative treatment modalities of native liver diseases. In this review article, the potential causes and histopathological features of late allograft dysfunction are discussed. The causes include recurrence of native liver disease, late-onset acute rejection, chronic rejection, and posttransplant malignancy or hepatitis of unknown etiology. Differential diagnosis between recurrent or late-onset acute rejection and early-stage chronic rejection, either reversible or finally leading to late-stage chronic rejection, is practically difficult; however, clinically, it affects patient treatment. Diagnosis of recurrent hepatitis B virus/hepatitis C virus hepatitis should be made with consideration of both serological evaluation for deoxyribonucleic acid, ribo nucleic acid, or antibodies and histopathological features. Although differentiation of recurrent or de novo autoimmune hepatitis from acute rejection is difficult, patients with autoimmune hepatitis undergo similar treatment. In pediatric patients, evaluation of Epstein-Barr virus-associated changes, which vary from nonspecific hepatitis to post- transplant lymphoproliferative disorder with or without acute rejection, is practically important from the point of treatment. From our 16-year experience in Asan Medical Center, it has become clear that the histopathological diagnosis of late allograft biopsies must be made on the basis of consensus criteria for the common and problematic causes of late complications of liver transplantations proposed by the Banff Working Group, by integration of clinical features and results of key serological tests, and even by consideration of responses to previous treatment.
Keyword
MeSH Terms
Figure
Reference
-
1). Desai M, Neuberger J. Chronic liver allograft dysfunction. Transplant Proc. 2009; 41:773–6.
Article2). European Liver Transplant Registry (ELTR). Overall in-dication and results [Internet]. Villejuif: ELTR;2013. [cited 2013 Nov 10]. Available from. http://www.eltr.org.3). Banff Working G, Demetris AJ, Adeyi O, Bellamy CO, Clouston A, Charlotte F, et al. Liver biopsy interpretation for causes of late liver allograft dysfunction. Hepatology. 2006; 44:489–501.
Article4). Hübscher SG. What is the long-term outcome of the liver allograft? J Hepatol. 2011; 55:702–17.
Article5). Anand AC, Hubscher SG, Gunson BK, McMaster P, Neuberger JM. Timing, significance, and prognosis of late acute liver allograft rejection. Transplantation. 1995; 60:1098–103.
Article6). Hübscher SG. Central perivenulitis: a common and po-tentially important finding in late posttransplant liver biopsies. Liver Transpl. 2008; 14:596–600.
Article7). Wiesner RH, Batts KP, Krom RA. Evolving concepts in the diagnosis, pathogenesis, and treatment of chronic hepatic allograft rejection. Liver Transpl Surg. 1999; 5:388–400.
Article8). Demetris A, Adams D, Bellamy C, Blakolmer K, Clouston A, Dhillon AP, et al. Update of the International Banff Schema for Liver Allograft Rejection: working recom-mendations for the histopathologic staging and reporting of chronic rejection. An International Panel. Hepatology. 2000; 31:792–9.9). O'Grady JG. Phenotypic expression of recurrent disease after liver transplantation. Am J Transplant. 2010; 10:1149–54.10). Burt AD, Portmann BC, et al. MacSween's pathology of the liver. 6th ed.Edingurgh: Churchill Livinstone;2012.11). Campos-Varela I, Castells L, Buti M, Vargas V, Bilbao I, Rodríguez-Frías F, et al. Does pre-liver transplant HBV DNA level affect HBV recurrence or survival in liver transplant recipients receiving HBIg and nucleos(t)ide analogues? Ann Hepatol. 2011; 10:180–7.
Article12). Petrovic LM. Recurrent diseases following liver transplantation: current concepts. Curr Opin Organ Transplant. 2012; 17:293–302.13). Rubín A, Aguilera V, Berenguer M. Liver transplantation and hepatitis C. Clin Res Hepatol Gastroenterol. 2011; 35:805–12.14). Samonakis DN, Germani G, Burroughs AK. Immuno-suppression and HCV recurrence after liver transplantation. J Hepatol. 2012; 56:973–83.
Article15). Demetris AJ. Evolution of hepatitis C virus in liver allografts. Liver Transpl. 2009; 15(Suppl 2):S35–41.
Article16). Narang TK, Ahrens W, Russo MW. Post-liver transplant cholestatic hepatitis C: a systematic review of clinical and pathological findings and application of consensus criteria. Liver Transpl. 2010; 16:1228–35.
Article17). Berardi S, Lodato F, Gramenzi A, D'Errico A, Lenzi M, Bontadini A, et al. High incidence of allograft dysfunction in liver transplanted patients treated with pegy-lated-interferon alpha-2b and ribavirin for hepatitis C recurrence: possible de novo autoimmune hepatitis? Gut. 2007; 56:237–42.
Article18). Merli M, Gentili F, Giusto M, Attili AF, Corradini SG, Mennini G, et al. Immune-mediated liver dysfunction after antiviral treatment in liver transplanted patients with hepatitis C: allo or autoimmune de novo hepatitis? Dig Liver Dis. 2009; 41:345–9.
Article19). Khettry U, Huang WY, Simpson MA, Pomfret EA, Pomposelli JJ, Lewis WD, et al. Patterns of recurrent hepatitis C after liver transplantation in a recent cohort of patients. Hum Pathol. 2007; 38:443–52.
Article20). Demetris AJ, Eghtesad B, Marcos A, Ruppert K, Nalesnik MA, Randhawa P, et al. Recurrent hepatitis C in liver allografts: prospective assessment of diagnostic accuracy, identification of pitfalls, and observations about pathogenesis. Am J Surg Pathol. 2004; 28:658–69.21). Krieger NR, Martinez OM, Krams SM, Cox K, So S, Esquivel CO. Significance of detecting Epstein-Barr-spe-cific sequences in the peripheral blood of asymptomatic pediatric liver transplant recipients. Liver Transpl. 2000; 6:62–6.
Article22). Kim SA, Song DE, Kim JH, Jang SJ, Jang JY, Kim KM, et al. Clinicopathologic analysis of explanted liver and allograft liver biopsy in pediatric patients. Korean J Pathol Suppl. 2008; 42:57.23). Pfitzmann R, Schwenzer J, Rayes N, Seehofer D, Neu-haus R, Nussler NC. Long-term survival and predictors of relapse after orthotopic liver transplantation for alco-holic liver disease. Liver Transpl. 2007; 13:197–205.
Article24). Kim WR, Poterucha JJ, Porayko MK, Dickson ER, Steers JL, Wiesner RH. Recurrence of nonalcoholic steatohepa-titis following liver transplantation. Transplantation. 1996; 62:1802–5.25). Riva S, Sonzogni A, Bravi M, Bertani A, Alessio MG, Candusso M, et al. Late graft dysfunction and autoantibodies after liver transplantation in children: preliminary results of an Italian experience. Liver Transpl. 2006; 12:573–7.
Article26). Cho JM, Kim KM, Oh SH, Lee YJ, Rhee KW, Yu E. De novo autoimmune hepatitis in Korean children after liver transplantation: a single institution's experience. Transplant Proc. 2011; 43:2394–6.
Article27). Salcedo M, Vaquero J, Bañares R, Rodríguez-Mahou M, Alvarez E, Vicario JL, et al. Response to steroids in de novo autoimmune hepatitis after liver transplantation. Hepatology. 2002; 35:349–56.
Article28). Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999; 31:929–38.
Article29). Mieli-Vergani G, Vergani D. De novo autoimmune hepatitis after liver transplantation. J Hepatol. 2004; 40:3–7.
Article30). Sebagh M, Castillo-Rama M, Azoulay D, Coilly A, Delvart V, Allard MA, et al. Histologic findings predictive of a diagnosis of de novo autoimmune hepatitis after liver transplantation in adults. Transplantation. 2013; 96:670–8.
Article31). Shaikh OS, Demetris AJ. Idiopathic posttransplantation hepatitis? Liver Transpl. 2007; 13:943–6.
Article32). Herzog D, Soglio DB, Fournet JC, Martin S, Marleau D, Alvarez F. Interface hepatitis is associated with a high incidence of late graft fibrosis in a group of tightly moni-tored pediatric orthotopic liver transplantation patients. Liver Transpl. 2008; 14:946–55.
Article33). Syn WK, Nightingale P, Gunson B, Hubscher SG, Neuberger JM. Natural history of unexplained chronic hepatitis after liver transplantation. Liver Transpl. 2007; 13:984–9.
Article34). Sebagh M, Rifai K, Feray C, Yilmaz F, Falissard B, Roche B, et al. All liver recipients benefit from the protocol 10-year liver biopsies. Hepatology. 2003; 37:1293–301.
Article35). Martin SR, Russo P, Dubois J, Alvarez F. Centrilobular fibrosis in long-term follow-up of pediatric liver transplant recipients. Transplantation. 2002; 74:828–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Histopathological Causes of Late Liver Allograft Dysfunction: Analysis at a Single Institution
- Histopathological findings of indication kidney allograft biopsy: 16-year experience from a tertiary care center in Korea
- Cardiac Allograft Injuries: A Review of Approaches to a Common Dilemma, With Emphasis on Emerging Techniques
- Characterization of Histopathological Features that Differentiate Hepatitis B Virus Infection from Acute Cellular Rejection
- Current safety and outcomes of kidney allograft biopsy