J Korean Soc Spine Surg.
2004 Sep;11(3):161-167. 10.4184/jkss.2004.11.3.161.
Prognostic Factors Associated with Revision Operation of Spine (Second Review)
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Busan, Korea. gylee@mail.donga.ac.kr
- KMID: 1839987
- DOI: http://doi.org/10.4184/jkss.2004.11.3.161
Abstract
- STUDY DESIGN: Patients who had had a revision operation were classified according to their outcome
OBJECTIVE
To review a consecutive series of patients who had had a revision operation on the lumbar spine and to determine which factors contributed to a successful outcome. SUMMARY OF LITERATURE REVIEW: The long-term failure rates after the primary surgery on the spine have been reported to be as high as 30 %. MATERALS AND METHODS: This study analyzed 57 patients who had had a revision operation on the lumbar spine between Sep-tember 1995 and December 2001, and had been followed for a minimum of two years and were available for analysis. All the patients had had a decompression and instrumented fusion except for two patients who had just undergone a bone graft. These patients were followed for an average of 39 months. There were 37 men and 20 women. The patients had undergone one or more surgical procedures and an average of 54 months had elapsed since the most recent operation. The average age at the time of the revision was 52 years. The outcome was considered to be successful if the patient had met the all three criteria (Ed note: What were the 3 criteria?). Several factors were evaluated using multiple regression (level of significance, P<0.05) to be determine which were related to a successful outcome.
RESULTS
Statistical analysis revealed that the factors associated with a successful outcome were a younger age (p<0.02), fewer spinal levels of revision surgery (p<0.05), pain-free interval after a previous operation (p<0.01). No significant relationship was observed between the outcome and gender, the number of prior procedures, the spinal level operated on, the presence of preoperative neurological signs and the intervals between the previous surgery and the revision.
CONCLUSION
These results suggest that the prognostic factors are useful for evaluating the successful outcome of revision surgery of the spine.
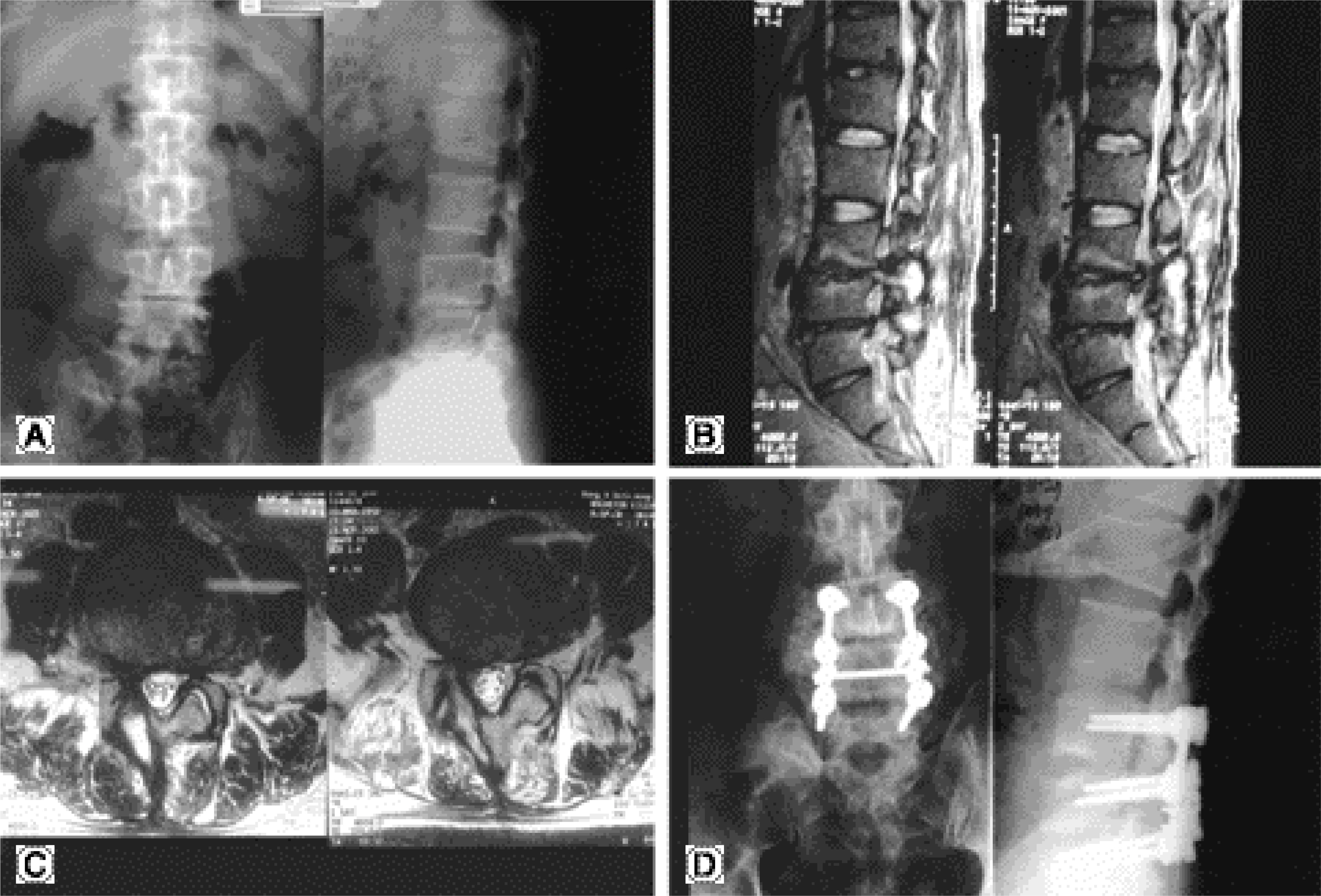
Figure
Reference
-
1). Bernard TN Jr. Repeat lumbar spine surgery. Factors influencing outcome. Spine. 1993; 18:2196–2200.2). Finnegan WJ, Fenlin JM, Marvei JP, Nardini RJ, Rothman RH. Results of surgical intervention in the symptomatic muliply-operated back patient. Analysis of sixty-seven cases followed for three to seven years. J Bone Joint Surg. 1979; 61-A:1077–1082.3). Kim SS, Michelsen CB. Revision surgery for failed back surgery syndrome. Spine. 1992; 17:957–960.
Article4). Lee KY, Sohn SK, Lee DH. Prognostic factors associated with revision operation of spine, J Kor Spine Surg. 2000; 7(1):53–60.5). Lehmann TR, LaRocca HS. Repeat lumbar surgery. A review of patients with failure from previous lumbar surgery treated by spinal canal exploration and lumbar spinal fusion. Spine. 1981; 6:615–619.6). Frymoyer JW, Hanley E. Howe J, Kuhlmann D, Mat-teri R. Disc excision and spine fusion in the management of lumbar disc disease. A minimum ten-year followup. Spine. 1978; 3:1–6.7). Frymoyer JW, Matterl RE, Hanley EN, Kuhimann D, Howe J. Failed lumbar disc surgery requiring second operation. A longterm followup study. Spine. 1978; 3:7–11.8). Cauchiox J, Ficat C, Girard B. Repeat surgery after disc excision. Spine. 1978; 3:256–259.
Article9). Crock HV. Observations on the management of failed spinal operations. J Bone Joint Surg. 1976; 58-B:193–199.
Article10). Saunders EA, Jacobs RR. The multiply operated back: fusion of the posterolateral spine with and without nerve root compression. Southern Med J. 1976; 69:868–871.11). Emery H, Paul MT. Postdecompression lumbar instability. Clin Orthop. 1988; 227:143–151.12). Suk SI, Lee JH, Min HJ, Kim HS, HA CH, Park SE. Salvage procedure in failed low back surgery. J Korean Orthop Assoc. 1993; 28(3):1009–1016.
Article13). Ha KY, Kim KW, Jang CH, Won JY. Multiply operated lumbar spine, J Kor Spine Surg. 1997; 4(2):329–336.14). Biondi J, Greenberg BJ. Redecompression and fusion in failed back syndrome patients. J Spinal Disorder. 1990; 3:362–369.15). Quimjian JD, Martka PJ. Decompression laminectomy and lateral spinal fusion in patients with previously failed lumbar spine surgery. Orthopedics. 1988; 11:563–569.
Article16). Waddell G, Kummel EG, Lotto WN, Graham JD, Hall H, McCulloch JA. Failed lumbar disc surgery and repeat surgery following industrial injuries. J Bone Joint Surg. 1979; 61-A:210–207.
Article17). Hurme M, Alaranta H. Factors predicting the result of surgery for lumbar intervertebral disc herniation. Spine. 1987; 12:933–938.
Article18). Spengler DM, Freeman C, Westbrook R, Miller JW. Low-back pain following multiple lumbar spine procedures. Failure of initial selection. Spine. 1980; 5:356–360.19). Blumenthal SL, Baker J, Dossett A, Selby DK. The role of anterior lumbar fusion for internal disc disruption. Spine. 1988; 13:566–569.
Article20). Crock HV. A reappraisal of intervertebral disc lesion. Med J Australia. 1970; 1:983–989.21). Froning EC, Frohman B. Motion of the lumbosacral spine after laminectomy and spine fusion. correlation of motion with the results. J Bone Joint Surg. 1968; 50-A:897–918.22). Longuidice VA, Johnson RG, Guyer RD, et al. Anterior lumbar interbody fusion. Spine. 1988; 13:366–369.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Factors Associated with Revision Operation of Spine
- The Revision Operation Rate for Adjacent Segmental Degeneration by Survival Analysis in Mono-segment Lumbar Fusion
- Complex Revision Surgery for Cervical Deformity or Implant Failure
- An Analysis of the Prognostic Factors Affecing the Clinical Outcomes of Conventional Lumbar Open Discectomy : Clinical and Radiological Prognostic Factors
- A Survival Analysis of Surgically Treated Metastatic Spine Tumors