J Korean Soc Radiol.
2014 Feb;70(2):137-143. 10.3348/jksr.2014.70.2.137.
Diagnosis of Benign and Metastatic Bone Lesions on Breast MRI in Patients with Breast Cancer
- Affiliations
-
- 1Department of Radiology, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea. escha@ewha.ac.kr
- KMID: 1839423
- DOI: http://doi.org/10.3348/jksr.2014.70.2.137
Abstract
- PURPOSE
To differentiate between the MRI findings for benign bone lesion and metastasis detected by breast MRI in patients with breast cancer and to evaluate the conspicuity of bone lesions according to MR sequences.
MATERIALS AND METHODS
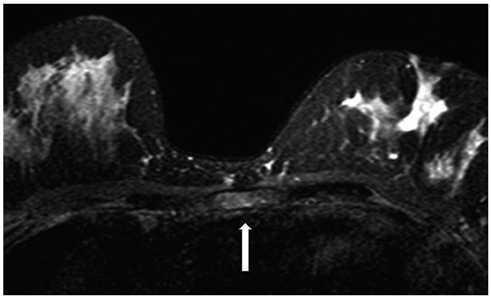
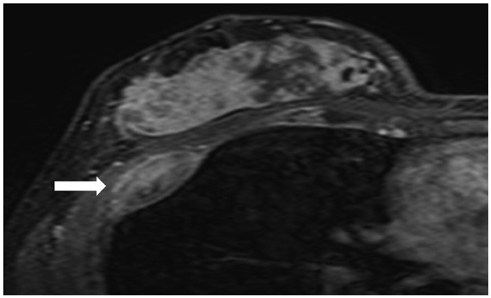
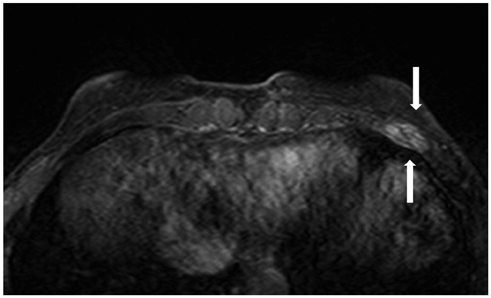
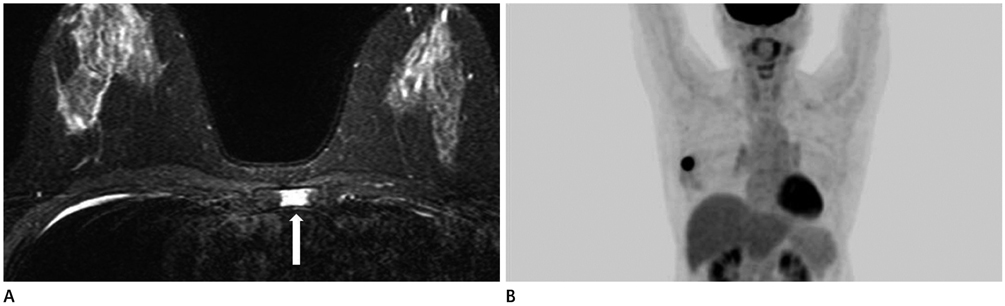
In 14 patients with 15 bone lesions, the MRI findings were statistically analyzed to differentiate between benign bone lesion and metastasis. We considered margin, signal intensity on T2-weighted image (T2WI) with spectral attenuated inversion recovery (SPAIR), enhancement, and patterns of bone lesions (focal mass, diffuse infiltration, and extraosseous soft tissue change), as well as the conspicuity of bone lesions in each MR sequence.
RESULTS
There was a statistically significant difference in the frequency of a solitary focal mass pattern between benign bone lesion and metastasis (p = 0.044). The margin, signal intensity on T2WI with SPAIR, and enhancement were not significantly different between benign bone lesion and metastasis. Both T2WI with SPAIR and delayed phase of contrast enhanced MRI were superior to other sequences in terms of lesion conspicuity.
CONCLUSION
A solitary focal mass pattern indicates a high probability of benign bone lesion on breast MRI in patients with breast cancer. Bone lesions tend to have greater conspicuity on T2WI with SPAIR and delayed phase image of contrast enhanced MRI, compared to results for other MR sequences.
Figure
Reference
-
1. Korean Breast Cancer Society. 2013 Breast cancer facts and figures. Seoul: Korean Breast Cancer Society;2013. 1:p. 4–13.2. Orel SG, Schnall MD. MR imaging of the breast for the detection, diagnosis, and staging of breast cancer. Radiology. 2001; 220:13–30.3. Schnall MD, Blume J, Bluemke DA, DeAngelis GA, DeBruhl N, Harms S, et al. Diagnostic architectural and dynamic features at breast MR imaging: multicenter study. Radiology. 2006; 238:42–53.4. Yabuuchi H, Kuroiwa T, Kusumoto C, Fukuya T, Ohno S, Hachitanda Y. Incidentally detected lesions on contrast-enhanced MR imaging in candidates for breast-conserving therapy: correlation between MR findings and histological diagnosis. J Magn Reson Imaging. 2006; 23:486–492.5. Yabuuchi H, Matsuo Y, Okafuji T, Kamitani T, Soeda H, Setoguchi T, et al. Enhanced mass on contrast-enhanced breast MR imaging: lesion characterization using combination of dynamic contrast-enhanced and diffusion-weighted MR images. J Magn Reson Imaging. 2008; 28:1157–1165.6. Rausch DR. Spectrum of extra-mammary findings on breast MRI: a pictorial review. Breast J. 2008; 14:592–594.7. Rinaldi P, Costantini M, Belli P, Giuliani M, Bufi E, Fubelli R, et al. Extra-mammary findings in breast MRI. Eur Radiol. 2011; 21:2268–2276.8. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al. American Joint Committee on Cancer. AJCC Cancer Staging Manual. 6th ed. New York: Springer-Verlag;2002.9. Liu T, Cheng T, Xu W, Yan WL, Liu J, Yang HL. A meta-analysis of 18FDG-PET, MRI and bone scintigraphy for diagnosis of bone metastases in patients with breast cancer. Skeletal Radiol. 2011; 40:523–531.10. Li S, Sun F, Jin ZY, Xue HD, Li ML. Whole-body diffusion-weighted imaging: technical improvement and preliminary results. J Magn Reson Imaging. 2007; 26:1139–1144.11. Hu S, Lustig M, Chen AP, Crane J, Kerr A, Kelley DA, et al. Compressed sensing for resolution enhancement of hyperpolarized 13C flyback 3D-MRSI. J Magn Reson. 2008; 192:258–264.12. Grankvist J, Fisker R, Iyer V, Fründ ET, Simonsen C, Christensen T, et al. MRI and PET/CT of patients with bone metastases from breast carcinoma. Eur J Radiol. 2012; 81:e13–e18.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Findings of Breast Diseases
- Clinical Outcome of Magnetic Resonance Imaging-Detected Additional Lesions in Breast Cancer Patients
- Clinical Applications of Breast MRI
- Application of Biomarkers for the Prediction and Diagnosis of Bone Metastasis in Breast Cancer
- Incidental Extramammary Findings on Preoperative Breast MRI in Breast Cancer Patients: A Pictorial Essay