Korean Circ J.
2009 Mar;39(3):124-127. 10.4070/kcj.2009.39.3.124.
Coronary Artery Thrombosis Associated With Paclitaxel in Advanced Ovarian Cancer
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. shinwy@schch.co.kr
- KMID: 1825971
- DOI: http://doi.org/10.4070/kcj.2009.39.3.124
Abstract
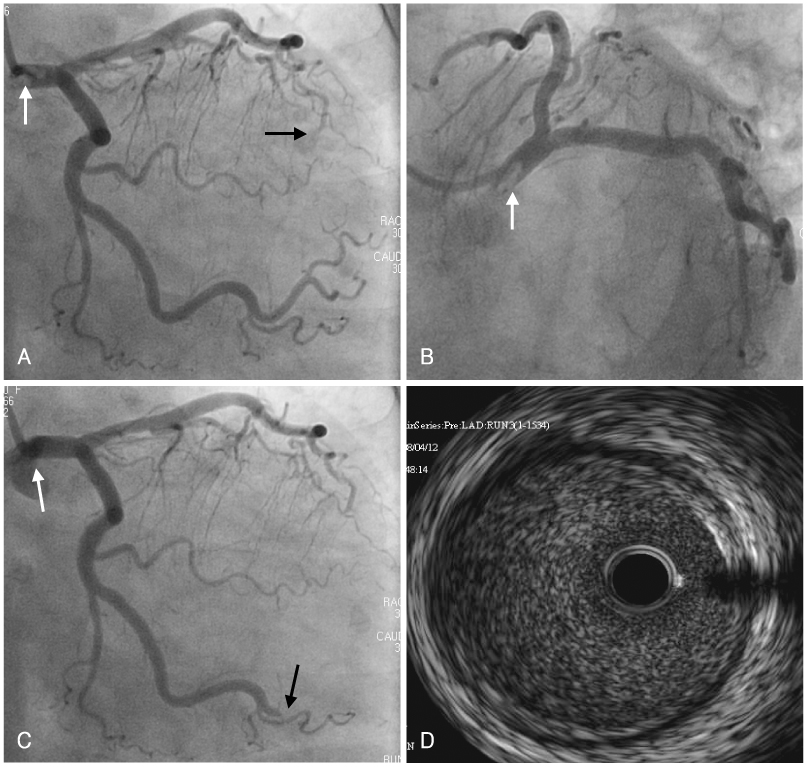
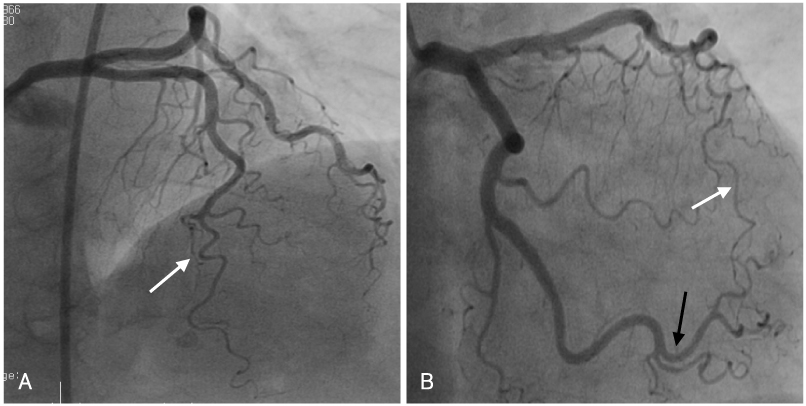
- A 63-year-old woman was diagnosed with ovarian cancer and peritoneal carcinomatosis. The day after paclitaxel was administered, an acute myocardial infarction occurred. Emergency coronary angiography revealed a filling defect in the left main coronary artery and total occlusion in the distal left anterior descending coronary artery, with no luminal irregularity or narrowing. Intravascular ultrasonography showed no significant plaque in the left main coronary artery. A thrombophilia work-up was negative, and the patient was treated with tirofiban, clopidogrel, and aspirin. The follow-up coronary angiogram showed that the occlusion of the distal obtuse marginal branch and distal left anterior descending artery had cleared. Paclitaxel has been associated with acute myocardial infarction. However, the pathogenesis of myocardial infarction associated with paclitaxel is not known. This case raises the possibility that paclitaxel can induce coronary artery thrombosis, resulting in myocardial infarction.
Keyword
MeSH Terms
-
Arteries
Aspirin
Carcinoma
Coronary Angiography
Coronary Thrombosis
Coronary Vessels
Emergencies
Female
Follow-Up Studies
Humans
Middle Aged
Myocardial Infarction
Ovarian Neoplasms
Paclitaxel
Phenobarbital
Thrombophilia
Thrombosis
Ticlopidine
Tyrosine
Ultrasonography, Interventional
Aspirin
Paclitaxel
Phenobarbital
Ticlopidine
Tyrosine
Figure
Reference
-
1. Kardasz I, De Carterina R. Myocardial infarction with normal coronary arteries: a conundrum with multiple aetiologies and variable prognosis: an update. J Intern Med. 2007. 261:330–348.2. Rowinsky EK, McGuire WP, Guarnieri T, Fisherman JS, Christian MC, Donehower RC. Cardiac disturbances during the administration of taxol. J Clin Oncol. 1991. 9:1704–1712.3. Selvanayagam JB, Iler MA, McRitchie RJ. Coronary thrombosis due to malignancy-induced thrombophilia. Intern Med J. 2002. 32:268–270.4. Rowinsky EK, Donehower RC. Paclitaxel (taxol). N Engl J Med. 1995. 332:1004–1014.5. Arbuck SG, Strauss H, Rowinsky E, et al. A reassessment of the cardiac toxicity associated with taxol. J Natl Cancer Inst Monogr. 1993. 15:117–130.6. Uhm JS, Park CS, Kim TS, et al. A case of acute myocardial infarction caused by coronary thrombus associated with a myocardial bridge and slow coronary flow. Korean Circ J. 2005. 35:639–642.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of advanced ovarian cancer which was treated with topotecan after taxol-cisplatin treatment failed
- A case of neoadjuvant chemotherapy with taxol / carboplatin in advanced epithelial ovarian cancer
- Weekly versus 3-weekly paclitaxel in combination with carboplatin in advanced ovarian cancer: which is the optimal adjuvant chemotherapy regimen?
- Acute Coronary Stent Thrombosis in Cancer Patients: A Case Series Report
- A Case of Paclitaxel Induced Scleroderma in a Patient with Ovarian Cancer