Peroral Endoscopic Myotomy for Treatment of Achalasia: Initial Results of a Korean Study
- Affiliations
-
- 1Institute for Digestive Research, Digestive Disease Center, Department of Internal Medicine, Soonchunhyang University Hospital, Soonchunhyang University College of Medicine, Seoul, Korea. cjy6695@dreamwiz.com
- 2Institute for Digestive Research, Digestive Disease Center, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- KMID: 1805298
- DOI: http://doi.org/10.5946/ce.2013.46.2.161
Abstract
- BACKGROUND/AIMS
Achalasia is a rare esophageal motility disorder. Recently, a novel endoscopic technique, peroral endoscopic myotomy (POEM), was introduced as an alternative treatment for achalasia. We report the results and short term outcomes of POEM for patients with achalasia.
METHODS
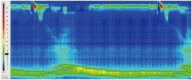
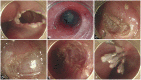
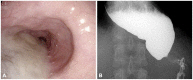
POEM was performed in 13 patients with achalasia. The procedure consisted of creating a submucosal tunnel followed by endoscopic myotomy of circular muscle bundles. The mucosal entry was closed by conventional hemostatic clips. A validated clinical symptom score (Eckardt score) and high resolution manometry were used to evaluate the outcomes.
RESULTS
Both the clinical score of achalasia, as well as the resting lower esophageal sphincter (LES) pressure, were significantly reduced after POEM. Mean posttreatment Eckardt score was 0.4+/-0.7, compared to 6.4+/-1.9 prior to the treatment (p=0.001). The mean pretreatment and posttreatment LES pressure was 30.3 and 15.3 mm Hg, respectively (p=0.007). Following POEM, symptomatic relief from dysphagia without reflux symptoms was observed in all patients (13/13). No serious complications related to POEM were encountered.
CONCLUSIONS
Based upon our initial experience, the authors believe that POEM is a feasible, safe, and effective treatment and may possibly substitute established treatments of refractory achalasia.
MeSH Terms
Figure
Cited by 6 articles
-
Jackhammer Esophagus Treated by a Peroral Endoscopic Myotomy
Weon Jin Ko, Byoung Moo Lee, Won Young Park, Jin Nyoung Kim, Jun-Hyung Cho, Tae Hee Lee, Su Jin Hong, Joo Young Cho
Korean J Gastroenterol. 2014;64(6):370-374. doi: 10.4166/kjg.2014.64.6.370.Current Status of Peroral Endoscopic Myotomy
Young Kwan Cho, Seong Hwan Kim
Clin Endosc. 2018;51(1):13-18. doi: 10.5946/ce.2017.165.Double-Scope Peroral Endoscopic Myotomy (POEM) for Esophageal Achalasia: The First Trial of a New Double-Scope POEM
Hee Jin Hong, Ga Won Song, Weon Jin Ko, Won Hee Kim, Ki Baik Hahm, Sung Pyo Hong, Joo Young Cho
Clin Endosc. 2016;49(4):383-386. doi: 10.5946/ce.2015.108.Highlights of International Digestive Endoscopy Network 2013
Kwang An Kwon, Il Ju Choi, Eun Young Kim, Seok Ho Dong, Ki Baik Hahm
Clin Endosc. 2013;46(5):425-435. doi: 10.5946/ce.2013.46.5.425.International Digestive Endoscopy Network 2014: Turnpike to the Future
Eun Young Kim, Kwang An Kwon, Il Ju Choi, Ji Kon Ryu, Ki Baik Hahm
Clin Endosc. 2014;47(5):371-382. doi: 10.5946/ce.2014.47.5.371.Peroral Endoscopic Myotomy: Establishing a New Program
Nikhil A. Kumta, Shivani Mehta, Prashant Kedia, Kristen Weaver, Reem Z. Sharaiha, Norio Fukami, Hitomi Minami, Fernando Casas, Monica Gaidhane, Arnon Lambroza, Michel Kahaleh
Clin Endosc. 2014;47(5):389-397. doi: 10.5946/ce.2014.47.5.389.
Reference
-
1. Achem SR, Crittenden J, Kolts B, Burton L. Long-term clinical and manometric follow-up of patients with nonspecific esophageal motor disorders. Am J Gastroenterol. 1992; 87:825–830. PMID: 1615935.2. Pehlivanov N, Pasricha PJ. Achalasia: botox, dilatation or laparoscopic surgery in 2006. Neurogastroenterol Motil. 2006; 18:799–804. PMID: 16918758.
Article3. Muehldorfer SM, Schneider TH, Hochberger J, Martus P, Hahn EG, Ell C. Esophageal achalasia: intrasphincteric injection of botulinum toxin A versus balloon dilation. Endoscopy. 1999; 31:517–521. PMID: 10533734.
Article4. Karamanolis G, Sgouros S, Karatzias G, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol. 2005; 100:270–274. PMID: 15667481.
Article5. Kilic A, Schuchert MJ, Pennathur A, Gilbert S, Landreneau RJ, Luketich JD. Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery. 2009; 146:826–831. PMID: 19789044.
Article6. Eldaif SM, Mutrie CJ, Rutledge WC, et al. The risk of esophageal resection after esophagomyotomy for achalasia. Ann Thorac Surg. 2009; 87:1558–1562. PMID: 19379905.
Article7. Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980; 26:8–10. PMID: 7358270.
Article8. Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007; 39:761–764. PMID: 17703382.
Article9. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010; 42:265–271. PMID: 20354937.
Article10. Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc. 2012; 26:3267–3272. PMID: 22609984.
Article11. von Renteln D, Inoue H, Minami H, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012; 107:411–417. PMID: 22068665.
Article12. Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010; 22:e256–e261. PMID: 20465592.
Article13. Hirano I, Tatum RP, Shi G, Sang Q, Joehl RJ, Kahrilas PJ. Manometric heterogeneity in patients with idiopathic achalasia. Gastroenterology. 2001; 120:789–798. PMID: 11231931.
Article15. Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008; 135:1526–1533. PMID: 18722376.
Article16. Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology. 2010; 139:369–374. PMID: 20600038.
Article17. Annese V, Bassotti G, Coccia G, et al. GISMAD Achalasia Study Group. A multicentre randomised study of intrasphincteric botulinum toxin in patients with oesophageal achalasia. Gut. 2000; 46:597–600. PMID: 10764700.
Article18. West RL, Hirsch DP, Bartelsman JF, et al. Long term results of pneumatic dilation in achalasia followed for more than 5 years. Am J Gastroenterol. 2002; 97:1346–1351. PMID: 12094848.
Article19. Hunter JG, Trus TL, Branum GD, Waring JP. Laparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg. 1997; 225:655–664. PMID: 9230806.
Article20. Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg. 2009; 249:45–57. PMID: 19106675.21. Richards WO, Torquati A, Holzman MD, et al. Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg. 2004; 240:405–412. PMID: 15319712.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Peroral Endoscopic Myotomy
- Perspective on Peroral Endoscopic Myotomy for Achalasia: Zhongshan Experience
- Two-Stage Peroral Endoscopic Myotomy for Sigmoid-Type Achalasia
- Peroral Endoscopic Myotomy for Esophageal Motility Disorders
- Double-Scope Peroral Endoscopic Myotomy (POEM) for Esophageal Achalasia: The First Trial of a New Double-Scope POEM